Anticoagulants: Warfarin vs. DOACs and Reversal Agents Explained
When you need to prevent dangerous blood clots-whether from atrial fibrillation, deep vein thrombosis, or a mechanical heart valve-choosing the right blood thinner isn’t just about effectiveness. It’s about safety, convenience, cost, and what happens if something goes wrong. For decades, warfarin was the only option. Today, DOACs (direct oral anticoagulants) are the go-to for most patients. But neither is perfect. And knowing how to reverse their effects in an emergency can mean the difference between life and death.
Why Blood Thinners Matter
Blood clots can kill. A clot in the leg can break loose and travel to the lungs, causing a pulmonary embolism. A clot in the heart can lead to stroke. Anticoagulants stop clots from forming or growing, but they don’t dissolve existing ones. That’s why they’re used long-term in people with atrial fibrillation, after a clot, or with certain artificial heart valves.Warfarin: The Old Standard
Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. That sounds simple, but it’s anything but. Warfarin’s effect is unpredictable. A small change in diet, another medication, or even a cold can throw your INR (International Normalized Ratio) out of range. Your INR needs to stay between 2.0 and 3.0 for most conditions. If it’s too low, you’re at risk for clots. Too high, and you risk bleeding. That means frequent blood tests-on average, 18 times a year. Some patients get tested every week. Many find this exhausting. It’s not just the needles. It’s the anxiety. The phone calls. The delays when you’re sick. Warfarin also interacts with hundreds of other drugs and foods. Green leafy vegetables? They’re full of vitamin K. Eating more than usual can make warfarin less effective. Antibiotics? They can make it stronger. Even over-the-counter pain relievers like ibuprofen can raise bleeding risk.DOACs: The New Generation
DOACs-like apixaban, rivaroxaban, dabigatran, and edoxaban-changed everything. They target specific parts of the clotting process directly. No vitamin K interference. No constant monitoring. No dietary restrictions. They start working within hours. They leave your system faster than warfarin. That means fewer drug interactions-only about 40 major ones per DOAC, compared to over 300 for warfarin. In large studies, DOACs reduced the risk of stroke and major bleeding by 17% to 35% compared to warfarin. Apixaban, in particular, showed a 35% drop in major bleeding. In 2023, 85% of new anticoagulant prescriptions in the U.S. were for DOACs. Academic hospitals use them as first-line for 89% of cases. Even Medicare beneficiaries prefer them-87% say they’d choose a DOAC over warfarin if given the choice.
When Warfarin Still Wins
DOACs aren’t for everyone. If you have a mechanical heart valve, DOACs are dangerous. They don’t work well here. Warfarin remains the only approved option. Severe kidney disease is another exception. DOACs are cleared by the kidneys. If your eGFR is below 15, they can build up to toxic levels. Warfarin doesn’t rely on kidney function, so it’s safer in end-stage renal disease. People with antiphospholipid syndrome-where the immune system attacks clotting proteins-also do better on warfarin. DOACs have higher rates of clot recurrence here. And then there’s cost. Warfarin costs $4 to $30 a month without insurance. DOACs? $300 to $500. Even with insurance, copays can be high. One in three Medicare patients skip doses because they can’t afford them. That’s a real risk.Reversal Agents: What Happens When You Bleed?
The biggest fear with any blood thinner is uncontrolled bleeding. A fall, a surgery, a stomach ulcer-any of these can turn deadly. With warfarin, you have tools. Vitamin K reverses it slowly over hours. Fresh frozen plasma gives you clotting factors but takes time to infuse. Prothrombin complex concentrate (PCC) works fast-often normalizing INR in under 30 minutes. These are widely available, even in small hospitals. DOACs don’t have universal reversal tools. But we do have targeted ones. For dabigatran, there’s idarucizumab (Praxbind®). It binds to the drug like a magnet and neutralizes it instantly. In studies, it reversed dabigatran in 98.7% of patients with major bleeding. But it costs $3,400 per vial. Not every hospital keeps it on hand. Only 62% of U.S. hospitals stock it. For rivaroxaban, apixaban, and edoxaban, there’s andexanet alfa (Andexxa®). It works like a decoy, soaking up the drug so it can’t interfere with clotting. It’s effective-but even pricier. A full treatment can cost $17,000. And it’s not always available outside big medical centers. If you don’t have access to a specific reversal agent, doctors use 4-factor PCC. It’s not as good, but it’s better than nothing. It works better for factor Xa inhibitors than for dabigatran. There’s hope on the horizon. Ciraparantag, an experimental universal reversal agent, is in Phase III trials. If approved, it could reverse all DOACs-and even heparin-with one drug. It’s not here yet, but it’s coming.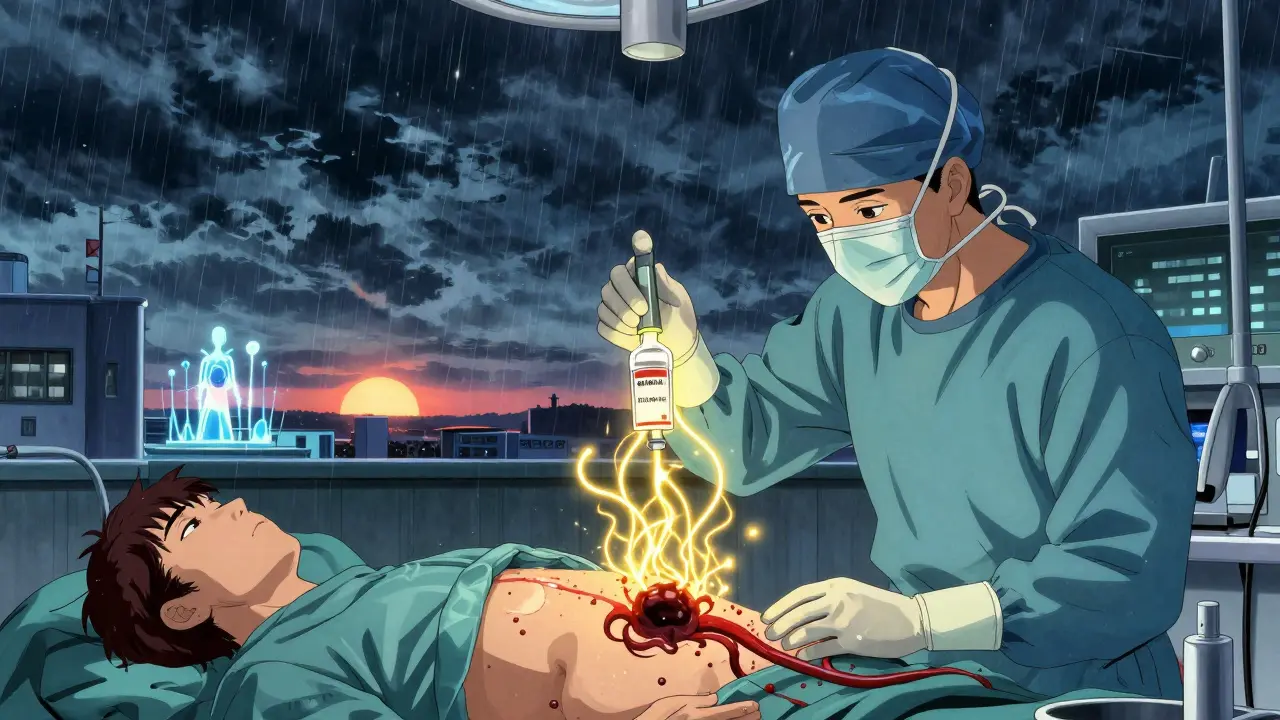
Who Gets Which Drug?
There’s no one-size-fits-all. Here’s how doctors decide:- Most patients with atrial fibrillation (no valve issues): DOACs first. Apixaban is often preferred because of its lower bleeding risk.
- Patients with mechanical heart valves: Warfarin only.
- Patients with severe kidney disease (eGFR <15): Warfarin.
- Patients with antiphospholipid syndrome: Warfarin.
- Patients who can’t afford DOACs: Warfarin-with strict monitoring.
- Patients who hate blood tests: DOACs.
- Patients over 80 or under 60kg: Lower-dose apixaban (2.5mg twice daily) is approved and often safer.

Ted Conerly
January 10, 2026 AT 11:01DOACs are a game-changer for most patients, no question. Less monitoring, fewer dietary nightmares, and solid data backing their safety. But let’s not pretend they’re perfect-cost and access to reversal agents are real barriers, especially in rural areas. We need better infrastructure before we declare warfarin obsolete.
Faith Edwards
January 11, 2026 AT 00:57How quaint. A man in his 50s, sipping chamomile tea while his INR wobbles like a drunk pendulum, still clings to warfarin like it’s a relic of moral virtue. Meanwhile, the rest of us live in the 21st century, where precision medicine isn’t a buzzword-it’s a lifeline. The fact that anyone still defends warfarin’s ‘character’ is less medical and more tragic.
Mario Bros
January 12, 2026 AT 03:06My grandma’s on apixaban and she hasn’t had a blood test in 2 years. She’s happier, healthier, and actually remembers to take her meds. Warfarin was a full-time job. DOACs? More like a reminder on her phone. 🙌
Ian Cheung
January 13, 2026 AT 09:15Cost is the elephant in the room nobody wants to name. I’ve seen patients skip doses because their copay’s $200 and they’re choosing between meds and groceries. DOACs aren’t magic if you can’t afford them. Warfarin’s cheap but the monitoring? That’s a hidden tax on your time and sanity. We need better policy not just better drugs
anthony martinez
January 14, 2026 AT 08:44So let me get this straight-you’re telling me we have a $17,000 drug to reverse another $500/month drug… and hospitals can’t always afford to stock it? Sounds like a corporate incentive model written by someone who’s never held a stethoscope.
Jay Amparo
January 14, 2026 AT 18:49As someone from a country where even basic anticoagulants are out of reach for most, I see this as a global privilege issue. DOACs are brilliant-but only if you live where the pharmacy has them, the hospital has reversal agents, and your insurance doesn’t make you beg. Warfarin isn’t outdated-it’s the only option for millions. We need equity, not just innovation.
Saumya Roy Chaudhuri
January 16, 2026 AT 13:14Anyone who still uses warfarin is either a medical dinosaur or hasn’t read a journal since 2010. DOACs have been in guidelines for over a decade. The data is ironclad. If your doctor still pushes warfarin, ask for a second opinion-preferably from someone who graduated after the Clinton administration.
Dwayne Dickson
January 17, 2026 AT 11:46While the clinical superiority of DOACs is well-documented, one must not conflate efficacy with accessibility. The pharmacoeconomic burden of reversal agents-particularly andexanet alfa-creates a tiered system of care wherein outcomes are dictated not by clinical need, but by institutional budgeting. This is not merely a therapeutic dilemma-it is a systemic failure of resource allocation in modern American healthcare.
Jake Nunez
January 19, 2026 AT 02:16My uncle had a GI bleed on warfarin. They gave him PCC and he was stable in 20 minutes. They tried to give him Praxbind for his DOAC bleed last year-hospital didn’t have it. Had to fly him 2 hours away. That’s not innovation. That’s a gamble.
Lisa Cozad
January 20, 2026 AT 17:41Just had a patient ask me if she could switch from warfarin to apixaban because she’s tired of getting poked every week. I said yes. She cried. Not from fear-from relief. Sometimes the best medicine isn’t the most advanced drug. It’s the one that lets you live your life.