Autoimmune Overlap: Understanding PBC, PSC, and AIH Combined Features

When your liver starts acting strange - fatigue that won’t quit, itchy skin, blood tests that don’t make sense - doctors usually look for one clear cause. But sometimes, it’s not just one disease. It’s two, or even three, hiding behind the same symptoms. This is what happens in autoimmune overlap syndromes, where features of Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC), and Autoimmune Hepatitis (AIH) mix together in the same person. It’s not rare. It’s not a fluke. And it’s not always easy to catch.
What Exactly Is an Autoimmune Liver Overlap?
Think of your liver as a factory. In healthy people, it runs smoothly. In autoimmune diseases, the body’s own immune system starts attacking parts of that factory. PBC targets the small bile ducts. PSC attacks the larger ones, causing scarring and blockages. AIH goes after the liver cells themselves. Each has its own signature: blood tests, antibodies, even how the tissue looks under a microscope.
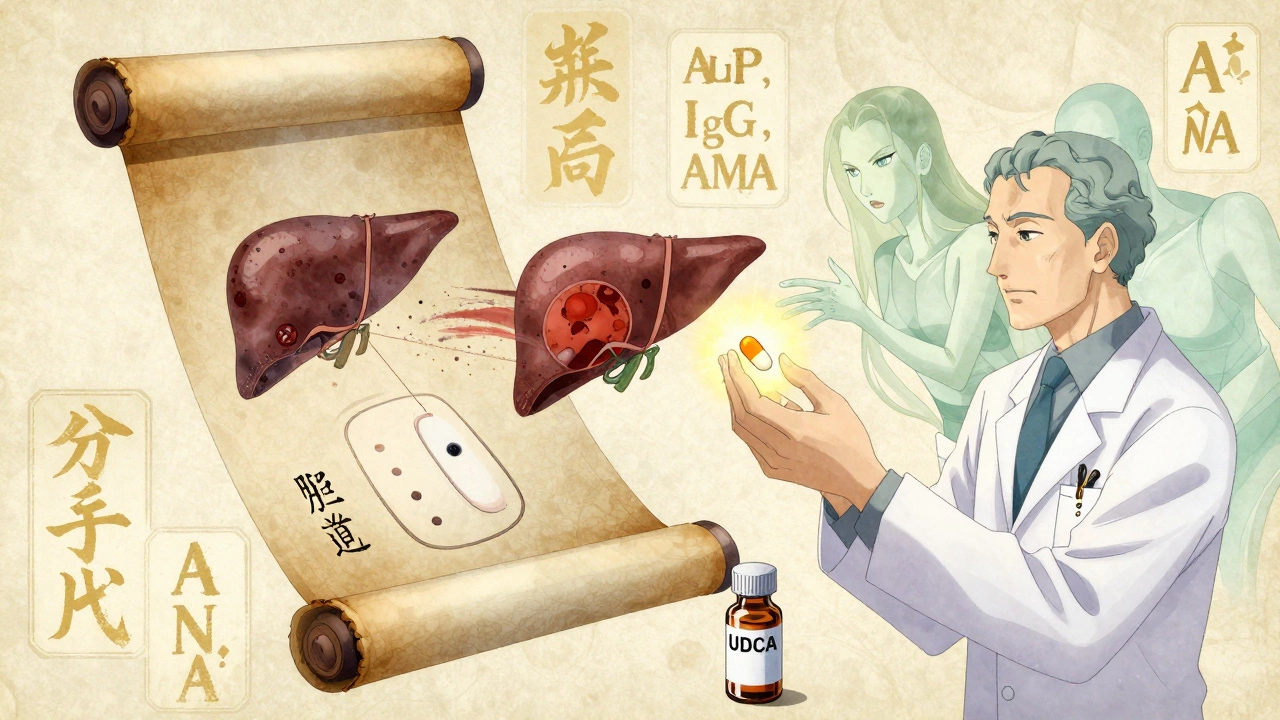
But in overlap syndromes, these signatures blur. A patient might have the high alkaline phosphatase of PBC, the elevated IgG and interface hepatitis of AIH, and maybe even some bile duct changes that look like PSC. The result? A confusing picture that doesn’t fit neatly into one box.
The most common overlap is AIH-PBC. Studies show it shows up in 1% to 3% of people with PBC - and up to 7% of those with AIH. Some larger studies even report numbers as high as 19%. That’s not small. It’s not rare. It’s a real clinical pattern that hepatologists see regularly, especially in middle-aged women - the same group most often affected by PBC and AIH.
How Do You Tell Them Apart?
Each disease has its fingerprint.
PBC usually hits women over 40. Blood tests show high ALP and GGT - signs of bile flow problems. The telltale sign? Anti-mitochondrial antibodies (AMA) in 90-95% of cases. Liver biopsy shows damaged small bile ducts, surrounded by immune cells. It progresses slowly, often over decades.
AIH can start at any age, but again, mostly in women. Here, ALT and AST are sky-high - meaning liver cells are being destroyed. IgG levels rise. You’ll see ANA or SMA antibodies. Under the microscope, there’s interface hepatitis: immune cells creeping into the liver tissue like invaders. Without treatment, cirrhosis can develop in years.
PSC is different. It’s more common in men, often linked to inflammatory bowel disease. ALP is high, but AMA is negative. MRIs show bumpy, beaded bile ducts - like a garden hose that’s been crushed in spots. Biopsies show concentric scarring around ducts. Unlike PBC, PSC doesn’t respond well to standard liver drugs.
Now, in overlap syndrome, you get a mix. A woman with AMA-positive PBC suddenly has her ALT jump. Her IgG climbs. A biopsy shows both bile duct damage and interface hepatitis. That’s AIH-PBC overlap. It’s not PBC getting worse - it’s something else adding on.
Why PBC-PSC Overlap Is Still a Mystery
There are case reports - single patients with features of both PBC and PSC. But experts still debate whether this is a real overlap or just two separate conditions happening by chance in the same person.
The problem? PBC and PSC don’t share the same immune triggers. PBC is tied to AMA and mitochondrial targets. PSC is linked to gut inflammation and unknown antigens. Their bile duct damage looks different under the microscope. No validated criteria exist for PBC-PSC overlap. Most major guidelines - from EASL and AASLD - say there’s no clear evidence it’s a true syndrome.
So if someone has both high ALP and bile duct changes on MRI, plus AMA positivity, doctors usually treat it as PBC with a side of PSC-like changes - not a new disease. The takeaway? Don’t assume PBC-PSC overlap. Look for something else first.

How Is It Diagnosed?
There’s no single test. No magic number. Diagnosis relies on putting together pieces from four areas: clinical symptoms, blood work, antibodies, and liver biopsy.
For AIH-PBC overlap, most experts use a simple rule: meet at least two of the three diagnostic criteria for both AIH and PBC.
For PBC, you need:
- ALP ≥ 1.5x upper limit of normal
- Positive AMA (or anti-sp100/gp210 if AMA-negative)
- Biopsy showing nonsuppurative cholangitis
For AIH, the International Autoimmune Hepatitis Group score looks at:
- Elevated IgG
- ANA or SMA
- Interface hepatitis on biopsy
- Other exclusion criteria (no alcohol, no viruses)
If a patient has AMA+, high ALP, and high IgG + interface hepatitis - that’s overlap. No need to wait for cirrhosis. No need to guess. The pieces fit.
But here’s the catch: many patients don’t get all the tests. A primary care doctor might see high ALP, order AMA, find it positive, and call it PBC. But if the ALT is also rising, and IgG is climbing? That’s a red flag. You need the full picture - including biopsy - to avoid missing AIH.
What Happens If You Treat It Wrong?
That’s where things get dangerous.
PBC is treated with ursodeoxycholic acid (UDCA). It’s safe, effective, slows progression. But if AIH is hiding underneath, UDCA alone won’t stop the immune system from attacking liver cells. The ALT stays high. Fibrosis keeps creeping in.
AIH is treated with steroids and azathioprine. But if you give those to someone with pure PBC, you risk side effects without benefit - and you might not touch the bile duct damage.
Overlap patients? They often need both.
Studies show 30-40% of AIH-PBC overlap patients don’t respond to UDCA alone. They need steroids or azathioprine added. Some need both drugs from the start. One 2020 case report described a 39-year-old man with asymptomatic enzyme elevations for six years. He was diagnosed with PBC, started on UDCA - but his ALT kept rising. Only after a biopsy showed interface hepatitis did doctors add prednisone. His enzymes normalized. His fibrosis stabilized.
Miss the overlap? You might think the PBC is progressing normally. But it’s actually the AIH doing damage - and you’re not treating it.
What’s the Long-Term Outlook?
Good news: if caught early and treated right, overlap syndromes don’t necessarily progress faster than single diseases.
Untreated, 30-40% of overlap patients develop cirrhosis within 10 years - similar to untreated AIH or PBC. But with combination therapy, many patients stabilize. Some even see improvement in liver enzymes and fibrosis.
Transplantation remains an option for end-stage disease - and outcomes are generally good. But post-transplant, recurrence patterns can differ. AIH can come back in the new liver. PBC less so. That’s why long-term monitoring is critical.
And yes - there’s still a small risk of liver cancer. That’s why regular ultrasounds and AFP blood tests are part of follow-up, even after treatment starts.
Why This Matters for Patients
If you’ve been told you have PBC - but you’re still tired, your ALT won’t drop, or you’re getting joint pain - ask: could there be more going on?
If you’ve been diagnosed with AIH - but your ALP is high and you have AMA - don’t assume it’s just AIH. Could PBC be hiding?
Many patients go years without a full workup. A single blood test. A biopsy skipped because “AMA is positive, so it’s PBC.” That’s not enough.
What you need:
- Full liver panel: ALT, AST, ALP, GGT, bilirubin, albumin, INR
- Autoantibodies: AMA, ANA, SMA, anti-sp100, anti-gp210
- IgG, IgM levels
- Liver biopsy - if any feature seems inconsistent
- MRCP or ultrasound to rule out PSC
Don’t let a simple label stop you from asking for more. You’re not just a diagnosis. You’re a person with a complex system - and your liver deserves a full picture.
What’s Next in Research?
Doctors are starting to think of autoimmune liver diseases not as separate boxes, but as a spectrum. AIH, PBC, PSC - they might be different points on one continuum. Overlap syndromes aren’t anomalies. They’re clues.
New autoantibodies are being discovered. Genetic markers are being studied. Clinical trials are underway to validate diagnostic criteria for overlap syndromes - with results expected by 2025.
For now, the message is clear: if the story doesn’t add up, look deeper. The liver doesn’t lie. But sometimes, it whispers - and you have to listen closely.

Donna Anderson
December 11, 2025 AT 20:23OMG this is SO real i had this exact thing happen to me and my doc just called it PBC and left it at that for 2 years until i lost my hair and my joints felt like glass 🤯
Lawrence Armstrong
December 13, 2025 AT 19:00Interesting breakdown. The key is that AMA positivity doesn't rule out AIH - I've seen patients with both who responded poorly to UDCA alone. Biopsy is non-negotiable if ALT/IgG are off. Many GPs miss this because they rely on one marker.
Also, the 19% overlap stat from that 2018 European cohort study is underreported. Real-world clinics see it more often than papers admit.
sandeep sanigarapu
December 13, 2025 AT 19:35Thank you for this clear explanation. Many patients are misdiagnosed because doctors rely on single tests. Liver biopsy remains essential. Always ask for full panel and antibodies. Your liver deserves nothing less.
Reshma Sinha
December 15, 2025 AT 06:21From a hepatology standpoint, the diagnostic criteria for AIH-PBC overlap are well-established per the IAHG and EASL consensus. The challenge lies in phenotypic heterogeneity and delayed biopsy referral. Biomarkers like anti-gp210 and anti-sp100 are underutilized in primary care settings, leading to therapeutic inertia. Combination therapy with UDCA + azathioprine demonstrates superior biochemical response over monotherapy in longitudinal cohorts. Early intervention prevents fibrotic progression and reduces transplant burden.
Robert Webb
December 16, 2025 AT 09:52I've been following autoimmune liver diseases for over a decade, both professionally and personally (my sister has AIH-PBC overlap). What really struck me is how the medical system tends to box things into neat categories, but the body doesn't work that way.
It's not just about the antibodies or the biopsy - it's about the whole person. Fatigue isn't just 'normal for PBC.' Joint pain isn't 'just aging.' The fact that some patients go years without a full workup because 'AMA is positive' is heartbreaking.
Doctors need to listen more than they need to label. And patients need to advocate for the full picture - even if it means pushing back. Your liver isn't a checklist. It's a living organ that's trying to tell you something. Sometimes it whispers. Sometimes it screams. But if you don't pay attention, it'll just stop talking altogether.
Ashley Skipp
December 17, 2025 AT 03:54So you're saying if you have AMA and high ALT you need steroids but they give you UDCA and call it a day what a joke
Levi Cooper
December 18, 2025 AT 13:56Why is this even a thing? In my country we don't have this confusion. We test once, treat once. No guessing games. Why are American doctors overcomplicating everything? It's just liver disease. Give the drug and move on.
Nathan Fatal
December 19, 2025 AT 02:58What fascinates me is how this reflects a deeper truth about medicine: we're trained to classify, but biology is a gradient. AIH, PBC, PSC aren't distinct boxes - they're nodes on a spectrum of immune dysregulation. The overlap syndromes aren't exceptions. They're the rule we're too lazy to admit.
Maybe the real question isn't how to diagnose overlap, but why we still cling to siloed categories when the evidence keeps pointing to a unified autoimmune landscape. The liver doesn't care about our diagnostic manuals. It only responds to what works.
Stacy Foster
December 19, 2025 AT 15:43Wait... so you're telling me the pharmaceutical companies knew about this all along? That's why UDCA is marketed as a 'cure' for PBC? They don't want you to know you might need steroids because it's cheaper to sell you one drug for life than two? And the guidelines? Written by people who get paid by drug reps. You think this is science? It's profit.
They're hiding this from you. They don't want you asking for biopsies. They don't want you demanding IgG tests. They want you on UDCA forever. And if you get cirrhosis? Well... that's when the transplant money starts flowing.
Don't trust your doctor. Don't trust the guidelines. Get your own biopsy. Demand the full panel. Or you're just another statistic in their quarterly report.