Breastfeeding Medication Timing: How to Reduce Infant Drug Exposure
Breastfeeding Medication Timing Calculator
Find the best time to take your medication to minimize your baby's exposure through breast milk.
Why Timing Your Medication Matters When You’re Breastfeeding
If you’re taking medication while breastfeeding, you’re not alone. Around 90% of nursing mothers use at least one prescription or over-the-counter drug in the first year after birth. But here’s the thing: when you take that pill can make a big difference in how much medicine your baby gets through your milk. It’s not about avoiding meds-it’s about using them smarter.
Many moms worry that any medication will harm their baby. But the truth is, most drugs pass into breast milk in tiny amounts. The real risk comes from timing. Take a painkiller right before feeding, and your baby gets the highest dose. Wait a few hours, and that dose drops by half-or even 75%. That’s not guesswork. It’s science.
How Drugs Move From Mom to Baby
Medications enter your breast milk the same way they enter your bloodstream: through your blood. When you swallow a pill, it gets absorbed, travels through your body, and ends up in your milk. The highest concentration in your milk usually happens 1 to 2 hours after you take it. That’s called the peak level.
Here’s what that looks like with common drugs:
- Morphine: Peaks in 30-60 minutes
- Oxycodone: Peaks in 30 minutes to 2 hours
- Codeine: Peaks in 60-90 minutes
- Tramadol: Peaks in 2-3 hours
- Acetaminophen: Peaks in 1 hour
- Ibuprofen: Peaks in 1-2 hours
After the peak, the drug slowly leaves your system. The time it takes for half of it to disappear is called the half-life. Morphine’s half-life is about 3 hours. Diazepam? Nearly 48 hours. That’s why timing matters more for short-acting drugs.
The Rule of Thumb: Feed Before You Take It
The most reliable strategy? Breastfeed your baby right before you take your medication. That way, your milk is at its lowest drug level when your baby feeds next.
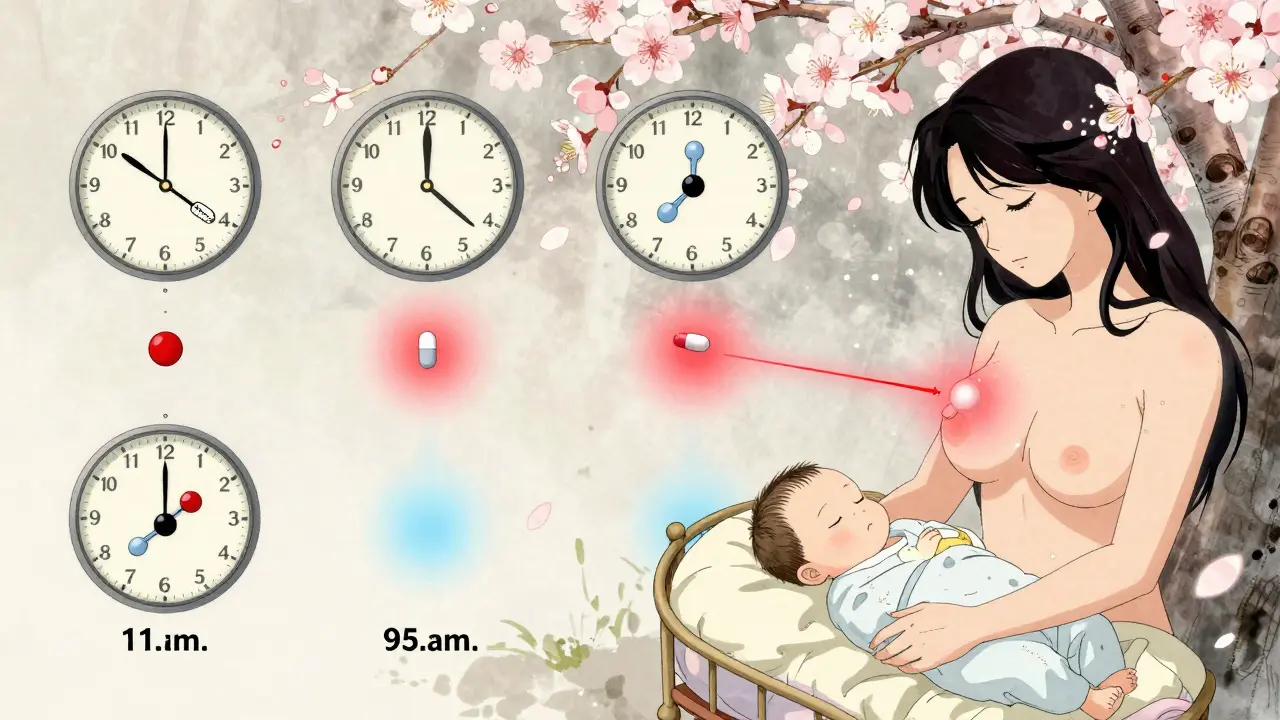
For example, if you take oxycodone for pain after a C-section:
- Feed your baby at 8 a.m.
- Take your pill at 9 a.m.
- Next feed is at 11 a.m.-by then, the drug level in your milk has dropped significantly.
- Wait until 2 p.m. for the next dose.
This simple shift can cut your baby’s exposure by 50-75%, according to the Academy of Breastfeeding Medicine (2022). It’s not magic. It’s just working with your body’s rhythm.
For long-acting drugs like diazepam or some antidepressants, timing doesn’t help as much. The drug stays in your system for days. In those cases, the focus shifts to using the lowest effective dose and choosing safer alternatives.
Which Medications Are Safest?
Not all meds are created equal. Some barely make it into your milk. Others? They’re risky no matter when you take them.
Here’s what experts recommend:
- Best choices: Acetaminophen and ibuprofen. Both have very low transfer rates. Your baby gets less than 1% of your dose. These are first-line for pain and fever.
- Use with caution: Opioids like hydrocodone and morphine. They’re okay if timed right and used short-term. Avoid codeine and tramadol entirely. The FDA warns these can cause dangerous breathing problems in babies, especially if you’re a fast metabolizer.
- Benzodiazepines: Alprazolam (Xanax) is shorter-acting than diazepam (Valium). If you need an anxiety med, go for alprazolam and time it after feeding. Avoid long-term use.
- Antidepressants: Sertraline and paroxetine are preferred. They’re low in milk and have decades of safety data. Avoid fluoxetine-it builds up in your baby’s system.
The American Academy of Pediatrics says: “The benefits of breastfeeding usually outweigh the risks of medication exposure.” But that only holds true if you pick the right drug and time it right.
What About Pumping and Dumping?
Most moms hear: “Pump and dump after your pill.” That’s outdated advice.
Here’s why: Pumping doesn’t remove the drug from your milk faster. It just removes milk that already contains the drug. Your body keeps making more. If you pump and dump right after taking a pill, you’re just wasting milk-and your body will replace it with more of the same drug.
There’s one exception: If you’re taking a medication you’ve been told to avoid entirely (like certain chemotherapy drugs), then pumping and dumping helps maintain your supply while you wait for the drug to clear. But for most common meds, it’s unnecessary.
Instead, plan ahead. If you know you’ll need a painkiller after surgery, pump and store milk a few hours before your procedure. That way, you have safe milk ready for your baby while you recover.
Special Cases: Newborns, Premies, and High-Risk Babies
Not all babies react the same. Newborns, especially in the first 3-4 days, get very little medication through milk because they’re not drinking much. Your milk supply is low, and their livers are still learning how to process drugs.
But if your baby was born early, has liver or kidney issues, or is sick, they process drugs slower. That means even small amounts can build up. In these cases, timing becomes even more critical-and so does working with a specialist.
Always tell your doctor, pharmacist, or lactation consultant if your baby has health issues. They may recommend a different drug or adjust your dose.
What to Do If You’re Already Taking a Risky Med
If you’re on codeine, tramadol, or a long-acting benzodiazepine and didn’t know about timing, don’t panic. But do act.
- Stop the drug if you can, and switch to a safer option. Ask your doctor about alternatives.
- If you can’t stop, time your doses after feeding. Never take it right before a feed.
- Watch your baby closely for signs of drowsiness, trouble feeding, or slow breathing. If you see any, call your pediatrician immediately.
The FDA issued warnings on codeine and tramadol in 2017 and 2018 for a reason. These drugs have caused infant deaths. Timing won’t fix that risk. Safety comes from avoiding them altogether.

How to Get Personalized Advice
There’s no one-size-fits-all plan. Your medication, your metabolism, your baby’s age-all matter.
Start with your doctor. But if they’re unsure, ask for a lactation consultant or call the LactMed database (run by the U.S. National Library of Medicine). It’s free, updated quarterly, and has detailed info on over 1,000 medications.
Also, tell every provider you see-dentist, pharmacist, ER doctor-that you’re breastfeeding. Many don’t ask. But if you say it upfront, they’ll check before prescribing.
Real-Life Tips That Work
- Keep a schedule: Write down when you take meds and when you feed. Use a phone app or paper log. After a few days, you’ll see the pattern.
- Feed on demand: Newborns feed every 2-3 hours. That actually helps-you’re not stuck with one long gap. Use the natural rhythm to your advantage.
- Use immediate-release pills: They work fast and clear fast. Avoid extended-release versions. They keep the drug in your system longer, making timing useless.
- Don’t rush: It takes 1-2 weeks to get comfortable with timing. Be patient. Your body and your baby will adjust.
What’s Changing in 2026
Science is getting better at predicting how drugs behave in each person. Researchers are now testing for CYP2D6 gene variants-those tell us if you’re a fast or slow metabolizer of drugs like codeine and tramadol. In the future, your doctor might order a simple saliva test before prescribing.
Right now, 27 U.S. states include medication timing in Medicaid-covered breastfeeding support. New Zealand is catching up. More hospitals are training staff to give clear, practical advice-not just warnings.
The message is clear: You don’t have to choose between being a healthy mom and being a breastfeeding mom. With the right timing, you can do both.
Can I take ibuprofen while breastfeeding?
Yes, ibuprofen is one of the safest pain relievers for breastfeeding moms. Less than 1% of your dose gets into your milk, and it doesn’t build up in your baby’s system. Take it after a feeding to keep levels low. It’s recommended by the American Academy of Pediatrics and the Academy of Breastfeeding Medicine.
Is it safe to take Tylenol while breastfeeding?
Yes, acetaminophen (Tylenol) is considered very safe during breastfeeding. Only tiny amounts pass into breast milk, and no harmful effects have been reported in nursing infants. It’s often the first choice for pain or fever in new moms.
What should I do if my baby seems sleepy after I take painkillers?
If your baby is unusually sleepy, hard to wake for feeds, or has slow or shallow breathing, contact your pediatrician right away. These could be signs of opioid exposure. Stop the medication and ask for a safer alternative. Never ignore these symptoms.
Do I need to pump and dump after taking medication?
No, not for most medications. Pumping and dumping doesn’t speed up how fast the drug leaves your body. It just wastes milk. The best approach is to time your doses after feeding. Only pump and dump if you’re on a medication your doctor says is unsafe, and you need to maintain your supply while it clears.
Can I take anxiety meds like Xanax while breastfeeding?
Alprazolam (Xanax) can be used short-term while breastfeeding if timed correctly. Take it right after a feeding and wait at least 2-3 hours before the next one. Avoid long-term use. Diazepam (Valium) is riskier because it stays in your system for days. Talk to your doctor about sertraline or other SSRIs-they’re often safer for long-term use.
Are there any medications I should avoid completely while breastfeeding?
Yes. Codeine and tramadol are FDA warnings because they can cause life-threatening breathing problems in babies, especially in mothers who metabolize them quickly. Avoid these entirely. Also avoid certain antidepressants like fluoxetine, and any medication with a black box warning for infants. Always check LactMed or ask a lactation consultant before starting any new drug.
How do I know if a medication is safe for breastfeeding?
Check the LactMed database from the U.S. National Library of Medicine-it’s free and updated every three months. It gives you the relative infant dose (RID), peak levels, and timing advice. You can also ask your pharmacist or a certified lactation consultant. Never rely on internet forums or anecdotal advice.

christy lianto
January 8, 2026 AT 19:45Aubrey Mallory
January 9, 2026 AT 19:37Prakash Sharma
January 11, 2026 AT 17:20swati Thounaojam
January 12, 2026 AT 14:15Manish Kumar
January 12, 2026 AT 18:34Dave Old-Wolf
January 12, 2026 AT 19:45Donny Airlangga
January 12, 2026 AT 22:17Molly Silvernale
January 14, 2026 AT 22:06And yes, I cried reading this. Not because I was scared-but because someone finally said it without fear-mongering.
Kristina Felixita
January 15, 2026 AT 20:10Joanna Brancewicz
January 15, 2026 AT 23:18Evan Smith
January 17, 2026 AT 20:02Lois Li
January 19, 2026 AT 18:06Ken Porter
January 20, 2026 AT 04:21Annette Robinson
January 21, 2026 AT 00:08