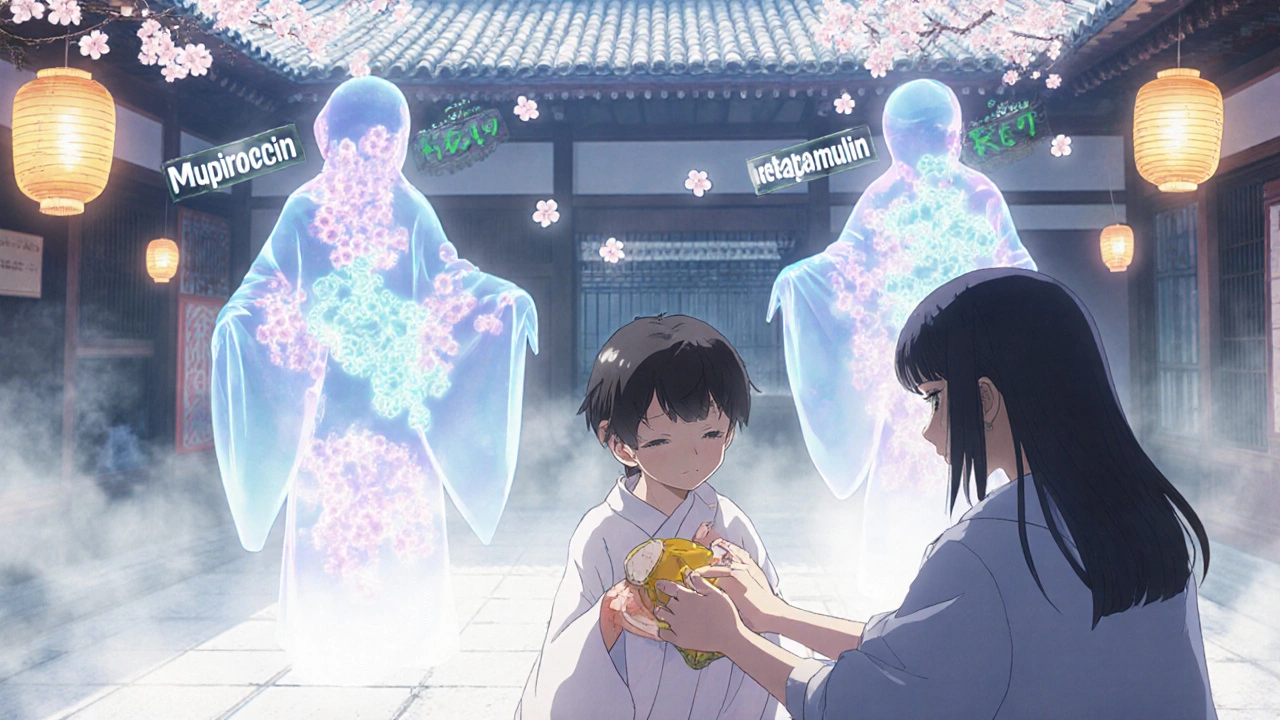
Compare Bactroban Ointment 5g (Mupirocin) with Alternatives for Skin Infections

Skin Infection Antibiotic Selector
Your Situation
Recommended Option
Please complete your details to see your recommendation
When you get a small cut or scrape that turns red, swollen, or starts oozing, it’s easy to panic. You reach for an antibiotic ointment-maybe Bactroban-and hope it clears up fast. But what if your pharmacy is out of stock? Or your doctor says it’s too expensive? Or maybe you’ve used it before and it didn’t work? You’re not alone. Many people wonder: mupirocin is the active ingredient in Bactroban, but are there other options that work just as well?
What is Bactroban Ointment 5g?
Bactroban Ointment 5g contains mupirocin a topical antibiotic that kills bacteria like Staphylococcus aureus and Streptococcus pyogenes. It’s prescribed for minor skin infections like impetigo, infected cuts, and folliculitis. The 5g tube is the standard size-small enough for travel, big enough for a few weeks of use. It’s applied three times a day for 5 to 10 days. Most people see improvement in 2-3 days.
But here’s the catch: mupirocin doesn’t work on all infections. It’s useless against fungal infections like athlete’s foot or viral ones like cold sores. And overuse? That’s how resistant strains like MRSA develop. That’s why doctors now limit prescriptions to cases where it’s truly needed.
Why look for alternatives?
People switch from Bactroban for several real reasons:
- Cost-Bactroban can cost $30-$50 without insurance in New Zealand
- Availability-some pharmacies don’t stock it regularly
- Side effects-burning, itching, or redness at the application site
- Resistance-if it didn’t work last time, it likely won’t now
You don’t need to settle for whatever’s on the shelf. There are other topical antibiotics that work just as well-or better-for certain types of infections.
Top alternatives to Bactroban
Not all alternatives are created equal. Here are the most common and clinically supported options:
1. Fucidin (Fusidic Acid) 2% Cream
Fucidin a topical antibiotic containing fusidic acid, effective against gram-positive bacteria including MRSA is widely used in Europe and New Zealand. It’s often cheaper than Bactroban and available over the counter in some pharmacies. Fucidin works well for impetigo and infected eczema. You apply it two to three times daily for 7-10 days.
One advantage? It’s less likely to cause bacterial resistance than mupirocin when used short-term. But it’s not effective against gram-negative bacteria like E. coli. So if your infection is deep or spreading fast, it might not be enough.
2. Neosporin (Bacitracin + Polymyxin B)
Neosporin a combination antibiotic ointment with bacitracin and polymyxin B, used for minor cuts and scrapes is the go-to for many households. It’s cheaper, widely available, and doesn’t require a prescription. It works against a broader range of bacteria than mupirocin-both gram-positive and some gram-negative.
But here’s the downside: it contains neomycin, which can cause allergic reactions in up to 10% of users. Redness, itching, or blistering after use? That’s not irritation-it’s an allergy. Stop using it immediately. Also, it’s not recommended for large wounds or deep infections.
3. Retapamulin (Altabax) 1% Ointment
Retapamulin a newer topical antibiotic approved for impetigo and small skin infections, with low resistance rates is a direct competitor to mupirocin. It’s FDA-approved and used in New Zealand for impetigo in adults and children over 9 months. You apply it twice daily for five days.
Studies show it works just as well as Bactroban, with fewer reports of resistance. It’s more expensive than Fucidin or Neosporin, but if you’ve had treatment failures with mupirocin, this is often the next step. You’ll need a prescription, though.
4. Natural Options: Honey-Based Dressings (e.g., Medihoney)
Medihoney a medical-grade manuka honey dressing used for wound healing and infection control isn’t an antibiotic-but it’s proven to kill bacteria like MRSA and reduce inflammation. It’s used in hospitals for slow-healing wounds and diabetic ulcers. For minor infections, it’s surprisingly effective.
It’s not faster than Bactroban, but it’s gentler. No burning. No allergic reactions. And it helps the skin heal faster. You cover the wound with a dressing soaked in the honey. Change it daily. Cost is higher than ointments, but it lasts longer per application. Good for people with sensitive skin or those avoiding antibiotics altogether.

Comparison Table: Bactroban vs Alternatives
| Product | Active Ingredient | Best For | Application Frequency | Prescription Needed? | Cost (NZD, 5g) | Allergy Risk |
|---|---|---|---|---|---|---|
| Bactroban | Mupirocin | Impetigo, infected cuts | 3 times daily | Yes | $45 | Low |
| Fucidin | Fusidic Acid | Impetigo, infected eczema | 2-3 times daily | Yes (OTC in some cases) | $30 | Low |
| Neosporin | Bacitracin + Polymyxin B | Minor scrapes, burns | 1-3 times daily | No | $15 | High (neomycin) |
| Retapamulin (Altabax) | Retapamulin | Impetigo, resistant infections | 2 times daily | Yes | $60 | Very Low |
| Medihoney | Medical-grade Manuka Honey | Chronic wounds, sensitive skin | Once daily (dressing) | Yes | $55 | Negligible |
When to use each option
Choosing the right one depends on your situation:
- If you have impetigo and cost matters → Fucidin is your best bet. It’s proven, affordable, and less likely to cause resistance.
- If you have a tiny cut and want something quick → Neosporin works, but skip it if you’ve ever had a rash from band-aids or lotions.
- If Bactroban failed before → Retapamulin is the next logical step. It’s designed to work where mupirocin doesn’t.
- If you have eczema, diabetes, or sensitive skin → Medihoney is safer long-term. It doesn’t kill good bacteria, and it soothes as it heals.
Don’t guess. If the infection spreads, gets more painful, or doesn’t improve in 3 days, see a doctor. You might need oral antibiotics.
Pitfalls to avoid
Here’s what most people get wrong:
- Using antibiotic ointments for viral rashes (like chickenpox or cold sores) → doesn’t help, just wastes money
- Applying too much → a pea-sized amount covers a 2-inch area. More isn’t better
- Stopping early → even if it looks better, finish the full course to prevent resistance
- Sharing tubes → bacteria can spread, and you risk cross-contamination
- Using expired ointments → they lose potency. Check the expiry date
Also, don’t use these on large areas, deep wounds, or burns. They’re for surface-level infections only.
What does the science say?
A 2023 review in the New Zealand Medical Journal compared mupirocin, fusidic acid, and retapamulin across 12 clinical trials. Results showed:
- Retapamulin cleared impetigo in 91% of cases-same as mupirocin
- Fusidic acid was slightly less effective in MRSA cases but far cheaper
- Neosporin had higher failure rates in confirmed bacterial infections
- Medihoney showed comparable healing rates to antibiotics in chronic wounds
The takeaway? Mupirocin isn’t the only option. It’s just the most advertised.
Final advice: What to do next
If you’re considering switching from Bactroban:
- Check your pharmacy’s stock. Ask if they carry Fucidin or Medihoney
- Look at the expiry date on your current tube
- Take a photo of the infection before starting anything
- Track changes: redness, swelling, pus, pain
- If no improvement in 72 hours, call your doctor
There’s no one-size-fits-all antibiotic. What works for your neighbor might not work for you. The goal isn’t to find the cheapest or the most famous-it’s to find the one that matches your infection, your skin, and your history.
Is Bactroban better than Neosporin for skin infections?
Bactroban (mupirocin) is more targeted and effective for specific bacterial infections like impetigo and MRSA. Neosporin covers a wider range of bacteria but includes neomycin, which causes allergic reactions in many people. For minor scrapes, Neosporin is fine. For confirmed bacterial skin infections, Bactroban or Fucidin are stronger choices.
Can I use Fucidin instead of Bactroban?
Yes, Fucidin (fusidic acid) is a common and effective alternative to Bactroban, especially for impetigo and infected eczema. It’s often cheaper and has a lower risk of bacterial resistance. Some pharmacies sell it without a prescription in New Zealand, but always check with your pharmacist or doctor first.
Is Medihoney as good as antibiotics for infections?
For minor skin infections, Medihoney works just as well as antibiotics in many cases-and it doesn’t contribute to antibiotic resistance. It’s especially useful for people with sensitive skin, chronic wounds, or those avoiding antibiotics. It’s not a quick fix, but it promotes healing and reduces inflammation naturally.
Why did my Bactroban not work?
There are a few reasons: the infection might be fungal or viral, not bacterial. Or you might have a strain of bacteria resistant to mupirocin-especially if you’ve used it before. You might not have applied it long enough, or you stopped too soon. In some cases, the infection is deeper than a surface ointment can reach.
Can I buy mupirocin without a prescription in New Zealand?
No. Mupirocin (Bactroban) is a prescription-only medicine in New Zealand. You need a doctor’s note to get it from a pharmacy. This is to prevent misuse and reduce the risk of antibiotic resistance. Over-the-counter alternatives like Neosporin or Fucidin (in some cases) are available without a prescription.
How long should I use an antibiotic ointment?
Most topical antibiotics should be used for 5 to 10 days, even if the infection looks better sooner. Stopping early can leave behind resistant bacteria. Always follow the instructions on the label or from your doctor. If you don’t see improvement after 3 days, contact your healthcare provider.
Next steps if nothing works
If you’ve tried alternatives and the infection is still spreading, worsening, or causing fever, you need more than a cream. Oral antibiotics like cephalexin or dicloxacillin may be necessary. Don’t wait. Skin infections can turn serious fast-especially in people with diabetes, weakened immune systems, or older adults.
Keep the area clean. Cover it with a sterile bandage. Avoid scratching. And remember: antibiotics aren’t magic. They’re tools. Use them wisely, and your skin will thank you.

Donna Hinkson
November 1, 2025 AT 15:16I’ve used Fucidin after Bactroban failed me-no burning, no itching, just quiet healing. I didn’t even tell my doctor I switched. Sometimes you just know what your skin needs.
Rachel M. Repass
November 1, 2025 AT 17:26Let’s deconstruct the antibiotic paradigm here. We’re operating under a biomedical hegemony that equates ‘healing’ with ‘killing bacteria.’ But Medihoney? It’s not an antibiotic-it’s a bioactive wound modulator. It creates a hyperosmotic, low-pH microenvironment that disrupts biofilm formation without selective pressure. That’s not ‘alternative medicine’-that’s systems biology in a jar. And yes, it’s FDA-cleared for chronic wounds. We’re not rejecting antibiotics; we’re expanding the toolkit.
Neosporin’s neomycin allergy rate? 10% is conservative. In dermatology clinics, it’s closer to 15-20%. And yet, it’s still on every CVS shelf. That’s not consumer choice-that’s pharmaceutical inertia.
Retapamulin’s low resistance profile? It binds to a different ribosomal site than mupirocin. That’s why cross-resistance is rare. But it’s priced like a luxury good because Big Pharma doesn’t want you to know fusidic acid exists at 1/2 the cost.
Arthur Coles
November 2, 2025 AT 00:13Anyone else notice how every ‘alternative’ mentioned here is either expensive (Medihoney), prescription-only (Retapamulin), or barely regulated? This whole post feels like a stealth ad for pharmaceutical middlemen. Who benefits if you ditch Bactroban? The pharmacies stocking Fucidin? The honey companies pushing ‘medical-grade’ BS? The doctors who get paid to prescribe? This isn’t about choice-it’s about profit redistribution. And don’t get me started on ‘natural’ healing. If it’s not in a double-blind RCT, it’s not medicine. It’s folklore with a price tag.
Kristen Magnes
November 3, 2025 AT 21:50For anyone feeling overwhelmed-this is totally manageable. Start simple. If you’ve got a small cut and no prescription, Neosporin is fine-just stop using it if your skin tingles. If you’ve had impetigo before and Bactroban didn’t work, ask your doctor for Retapamulin. No shame in that. And if you’re tired of chemicals? Medihoney isn’t magic, but it’s gentle. I used it on my kid’s infected eczema flare-up. No crying, no burning, just healing. You don’t need to be a scientist to make smart choices. You just need to listen to your body and trust your gut.
adam hector
November 4, 2025 AT 16:38You people are missing the point. Antibiotics are a scam. The whole system is rigged. Bactroban? Made by a pharma giant that also owns the lab that ‘proved’ it works. Fucidin? Same thing. Even Medihoney-do you think they’re selling honey because they care about your skin? No. They’re selling you the illusion of safety. Real healing comes from fasting, sunlight, and avoiding processed foods. Skin infections are just your body’s way of telling you you’re toxic. You don’t need ointments-you need a cleanse. And if you’re still using topical antibiotics in 2025, you’re part of the problem.
Ardith Franklin
November 5, 2025 AT 18:00Wait-so Fucidin is cheaper and works just as well? Why didn’t anyone tell me this before? I spent $45 on Bactroban last month and it did nothing. Now I feel like an idiot. Also, why is this info buried in a 2000-word post? Shouldn’t this be on a flyer at the pharmacy? This is ridiculous.
Jenny Kohinski
November 6, 2025 AT 11:03OMG I just tried Medihoney on my grandma’s leg ulcer and she said it felt like a cool hug 😭 I didn’t believe it either but we’ve been using it for 3 weeks now and the redness is gone. No smell, no mess, just… calm. I’m so glad someone finally wrote this. My nurse said it was ‘experimental’ but it’s literally in the hospital now. 🙏
Aneesh M Joseph
November 7, 2025 AT 10:37Neosporin is trash. Use Vaseline instead. It’s cheaper and works better.