Deprescribing Research: What Happens When You Reduce Medications in Older Adults
Medication Risk Assessment for Older Adults
This assessment helps you understand potential risks from your current medications. Based on the number of medications you take and whether you're using high-risk drugs, it identifies opportunities for safe deprescribing.
What This Means:
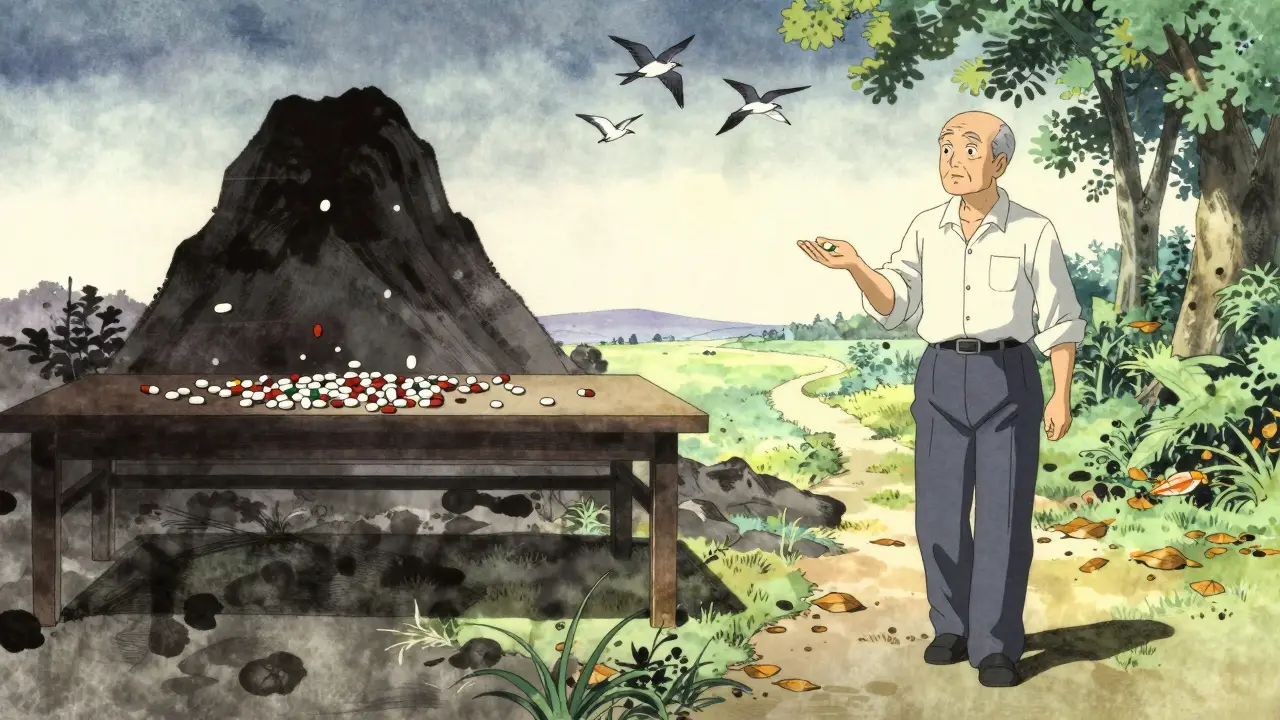
Every year, millions of older adults take more medications than they need. Some were prescribed years ago for a condition that’s since improved. Others were added to manage side effects from other drugs. Many are taken just because no one ever asked if they were still necessary. This isn’t laziness-it’s a systemic blind spot. And the consequences? Increased falls, confusion, hospital trips, and even early death. The good news? Deprescribing is changing that. It’s not about stopping meds randomly. It’s a careful, evidence-based process of removing drugs that no longer help-or worse, hurt.
What Exactly Is Deprescribing?
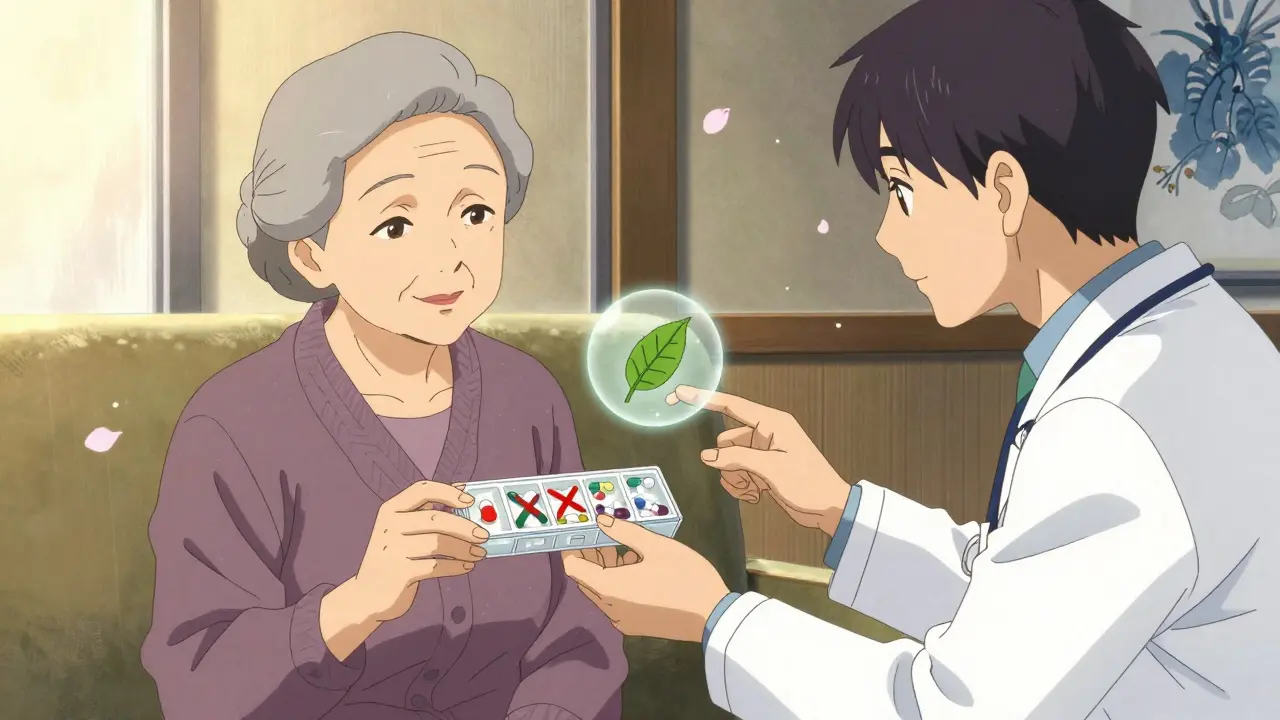
Deprescribing isn’t just cutting pills. It’s a planned, step-by-step process where doctors and patients work together to stop or reduce medicines that might be doing more harm than good. The definition is clear: Deprescribing is the systematic evaluation of whether the potential harms of a medication outweigh its benefits, based on a person’s current health, life expectancy, and personal goals. This approach was formalized around 2015, led by researchers in Canada and quickly adopted across North America. It’s now part of the American Geriatrics Society’s Beers Criteria, the gold standard for identifying risky drugs in older adults.Think of it like this: if you were told to take a pill every day for high blood pressure ten years ago, but your blood pressure is now normal and you’re frailer, that same pill might now be increasing your risk of fainting or kidney damage. Deprescribing asks: Is this drug still helping you live better today?
Who Benefits Most from Deprescribing?
Not everyone needs to cut back. But certain groups see the biggest gains:- Older adults taking five or more medications daily (about 40% of seniors in the U.S.)
- People with dementia or advanced frailty
- Those with terminal illness or limited life expectancy
- Patients who’ve had recent falls, confusion, or unexplained symptoms
- People on high-risk drugs like benzodiazepines (sleep aids), antipsychotics, or long-term proton pump inhibitors (heartburn drugs)
A 2023 study in JAMA Network Open found that community-dwelling seniors with polypharmacy had an average of 9.7 medications. After deprescribing interventions, that number dropped. Not by much per person-maybe one pill-but multiply that across a clinic of 2,000 patients, and you’re talking about 140 fewer drugs prescribed each year. That’s not just numbers. It’s fewer side effects, fewer ER visits, and more independence.
The Five Steps of a Safe Deprescribing Plan
You can’t just stop a pill cold turkey. Some medications cause dangerous withdrawal. Others need slow tapering. Here’s how professionals do it right:- Identify potentially inappropriate medications - Using tools like the Beers Criteria or STOPP/START guidelines, clinicians flag drugs with higher risks than benefits.
- Assess if reduction or stopping is possible - Is the drug still needed? Has the condition improved? Are there signs of side effects?
- Create a tapering plan - For drugs like antidepressants or blood pressure meds, doses are lowered slowly over weeks or months.
- Monitor closely - Patients are watched for symptoms like anxiety, insomnia, rebound pain, or blood pressure spikes. Some effects take weeks to show.
- Document everything - What was stopped? When? What happened? This helps avoid restarting drugs unnecessarily and informs future care.
One key rule? Stop one drug at a time. That way, if something changes-good or bad-you know which pill caused it.
What Do the Studies Say About Outcomes?
Early studies were mixed. Some showed no big difference in hospital visits or death rates. But here’s the catch: most were too short, too small, or only looked at medication counts-not real-life outcomes.Newer, better-designed research tells a clearer story. The Agency for Healthcare Research and Quality (AHRQ)’s PSNet reports that deprescribing leads to:
- Reduced risk of falls
- Improved mental clarity
- Lower hospital admission rates
- Fewer drug interactions
- Higher patient satisfaction
A 2024 study in the Journal of the American Geriatrics Society found that patients with multiple prescribers (like a cardiologist, neurologist, and GP) had the highest risk of harmful drug overlap. Deprescribing coordinated across providers cut those risks by over 30%.
And here’s something surprising: many patients want to take fewer pills. A survey by the American Academy of Family Physicians found that 8 out of 10 older adults would gladly reduce their meds-if their doctor brought it up. But only 1 in 5 ever had that conversation.
Why Don’t More Doctors Do It?
It’s not that they don’t care. It’s that the system doesn’t make it easy.- No time - A 15-minute appointment doesn’t leave room for a deep meds review.
- Lack of tools - Most electronic health records don’t flag risky combinations or suggest alternatives.
- Fear of backlash - Doctors worry patients will think they’re being neglected or that symptoms will return.
- No reimbursement - Insurance doesn’t pay for time spent reviewing meds unless it’s tied to a new diagnosis.
But things are shifting. Pilot programs in U.S. clinics using point-of-care deprescribing tools saw a 15% drop in inappropriate prescriptions. The Institute for Healthcare Improvement (IHI) now recommends a four-step rollout: assess current practices, set measurable goals, test changes in small groups, then scale up. Pharmacists are also stepping in-many now lead medication reviews in primary care teams.
What’s Next for Deprescribing?
The future isn’t just about stopping drugs-it’s about personalizing the process.- Genetic testing - Early research shows some people metabolize drugs like benzodiazepines or PPIs much slower due to genetics. Tailoring deprescribing to these profiles could make it safer.
- AI-assisted alerts - Health systems are testing algorithms that flag high-risk combinations during prescribing, suggesting alternatives.
- Shared decision-making tools - Apps and brochures from deprescribing.org (used over 500,000 times since 2015) help patients understand risks and ask informed questions.
- Long-term outcome studies - Experts like Dr. Dan Gnjidic are pushing for studies that track real results: falls, hospital stays, quality of life-not just pill counts.
By 2030, 20% of Americans will be over 65. Without action, polypharmacy will become a public health crisis. Deprescribing isn’t a fringe idea anymore. It’s becoming standard care.
What Can You Do?
If you or a loved one takes five or more daily medications:- Ask your doctor: “Which of these are still necessary?”
- Bring a full list of every pill, supplement, and OTC drug to your next visit.
- Ask: “What happens if I stop this? What are the risks vs. benefits?”
- Don’t be afraid to say: “I’d like to try taking fewer pills.”
Medications that helped five years ago might not be right for today. The goal isn’t to stop everything. It’s to make sure every pill you take is still working for you-not against you.
Is deprescribing safe?
Yes, when done properly. Studies show that most medications can be safely reduced or stopped under medical supervision. Withdrawal symptoms are rare and usually mild when tapering is slow and monitored. The bigger risk is continuing drugs that no longer help-and may be causing harm.
Can I stop my meds on my own?
No. Some medications, like antidepressants, blood pressure drugs, or steroids, can cause serious withdrawal effects if stopped suddenly. Always talk to your doctor first. Deprescribing is a planned process-not a DIY project.
What if my symptoms come back after stopping a drug?
Sometimes, symptoms return. That’s why monitoring is part of the process. If symptoms come back, your doctor may restart the drug at a lower dose, switch to a safer alternative, or investigate another cause. It’s not a failure-it’s part of finding the right balance.
Does deprescribing save money?
Yes. Reducing unnecessary prescriptions cuts pharmacy costs for individuals and health systems. One study estimated that a single primary care clinic could save over $10,000 annually by deprescribing just 50 unnecessary medications. That money can be redirected to higher-value care like physical therapy or mental health support.
Are there any medications that should never be stopped?
Not necessarily. Even drugs like aspirin or statins may be stopped if the patient’s life expectancy is short, or if risks now outweigh benefits. The decision isn’t based on drug class-it’s based on the individual. A 90-year-old with dementia and no history of heart disease likely doesn’t need daily aspirin. A 75-year-old with stable heart disease might.
