Double-Checking Medication Strength and Quantity Before Leaving the Pharmacy

Imagine picking up your child’s liquid antibiotic, handing it to them, and not realizing the pharmacy gave you 10 times the dose. That’s not a horror movie. That’s what happened to a mother in Ohio in 2022 because the pharmacist dispensed 5 mL instead of 0.5 mL - and gave her a teaspoon instead of an oral syringe. The child ended up in the hospital with liver damage. This isn’t rare. It happens because medication strength and quantity are checked too often as an afterthought, not a safety step.
Why This One Step Saves Lives
Pharmacists don’t just count pills. They verify the total amount of drug in the bottle, the concentration per milliliter, and whether the label matches the prescription. A simple mistake - like confusing 0.5 mg with 5 mg - can kill. The FDA says 63% of fatal medication errors involve high-alert drugs like insulin, opioids, and blood thinners. Most of these errors happen because no one stopped to ask: Is this the right amount in the container? The Institute for Safe Medication Practices (ISMP) made this a formal best practice in 2018. By 2023, they updated their guidelines to say: Never assume the strength on the label is the total amount. That’s because labels often show two numbers: the concentration (e.g., 10 mg/mL) and the total volume (e.g., 30 mL). If you misread the first as the total, you think the bottle has 10 mg - when it actually has 300 mg. That’s a 30-fold overdose.How It’s Done Right
There’s no magic trick. It’s a repeatable process. Here’s what a proper double-check looks like:- Look at the prescription. What did the doctor order? 5 mg? 10 mL? 250 mg total?
- Open the container. Read the label. What’s the strength per mL? What’s the total volume?
- Multiply. If it’s 10 mg/mL and 30 mL, that’s 300 mg total. Does that match the prescription?
- Check the dosing device. Did they give a teaspoon? A syringe? The right one?
- Confirm with a second person. Not just a nod. A verbal recalculation.
Why Visual Checks Aren’t Enough
You might think, “I just look at the bottle - it looks right.” But that’s how mistakes slip through. A 2021 study found visual checks alone catch only 38% of errors. Why? Because the human brain fills in gaps. If you see “10 mg/mL” and the bottle says “30 mL,” your brain might think “10 mg” is the total. It’s a cognitive trap. The FDA found that 64% of labeling errors involve decimal points. One misplaced decimal - 0.1 instead of 1.0 - can mean a tenfold overdose. That’s why USP <7> rules now require strength per total volume to be in a larger font than concentration. If the label doesn’t follow this, it’s not just sloppy - it’s dangerous.
What Happens When You Skip It
In 2023, a Reddit user shared a story from a pharmacy where staff skipped double-checks during a staffing crisis. A patient got 10 times their levothyroxine dose. They were hospitalized. That’s not a “mistake.” That’s a preventable event. And it’s not rare. Community pharmacies with fewer than five staff members are twice as likely to skip verification. Why? Pressure. Corporate rules push techs to process 35+ prescriptions per hour. That’s less than two minutes per script. No one can do a full calculation, check the device, and counsel the patient in that time. And patients? They’re not trained to question labels. A parent might think a teaspoon is safe. But 93% of pediatric dosing errors come from mixing up teaspoons and milliliters. That’s why ISMP and the FDA now demand metric-only dosing devices - oral syringes, not spoons.The Right Tools Make All the Difference
You can’t fix a system with bad tools. If the pharmacy gives you a measuring cup labeled “1 tsp = 5 mL,” but the prescription says 2.5 mL, you’re set up to fail. The right tools cost pennies: an oral syringe for $0.85, a calibrated dosing cup for $1.20. But many pharmacies still hand out spoons because they’re “cheaper” or “familiar.” The data is clear: pharmacies using metric-only devices reduce pediatric dosing errors by 41%. When paired with independent verification, the error rate drops even further. One study showed 94% of strength errors were caught when two people recalculated the dose - not just looked at it.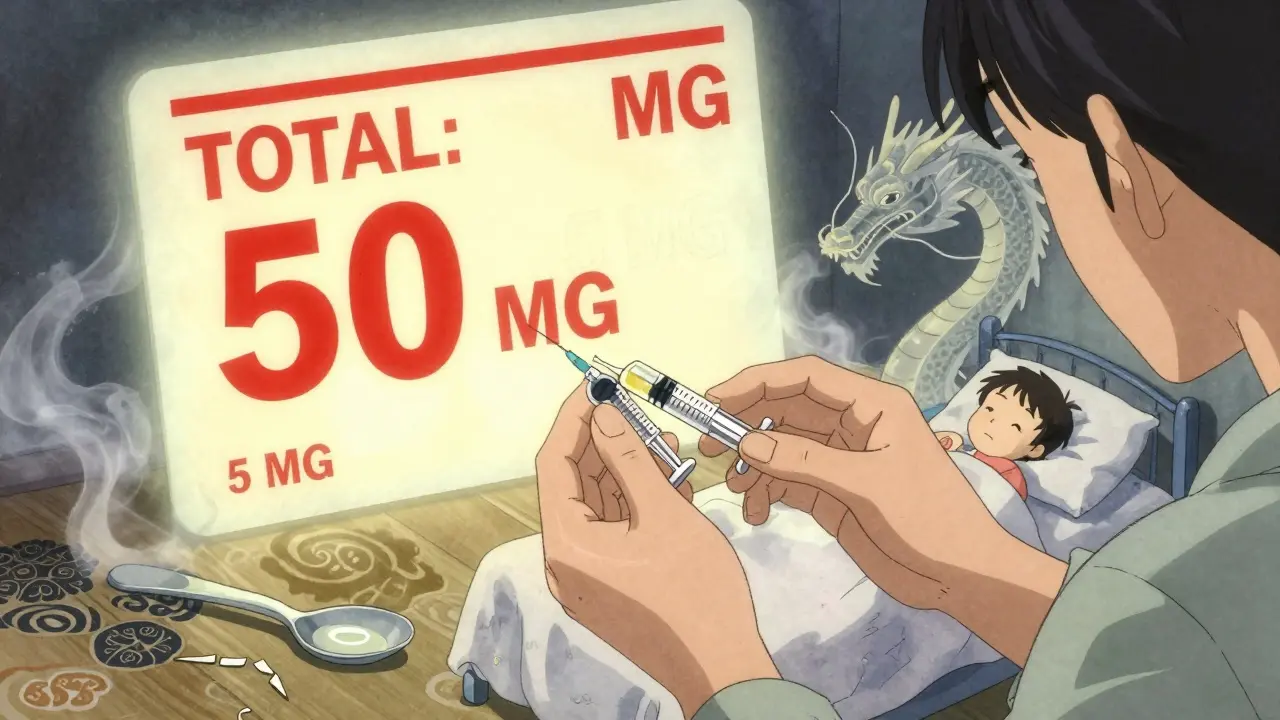
What You Can Do
You’re not powerless. Even if the pharmacy doesn’t have a formal double-check, you can protect yourself:- Always ask: “What’s the total amount in this bottle?”
- Ask: “Is this measured in milliliters or teaspoons?”
- Ask: “Can I get an oral syringe instead of a spoon?”
- Do the math: If it’s 5 mg/mL and the bottle says 10 mL, that’s 50 mg total. Does that match what your doctor ordered?
The Future Is Digital
Barcode scanning cuts dispensing errors by 83%. But it’s expensive - $15,000 to $25,000 per pharmacy. That’s why many small shops still rely on human checks. But change is coming. The FDA’s 2023 draft guidance requires all injectable labels to show the total drug amount in bold, oversized font by 2025. E-prescribing systems now must display the total dose prominently. And in 2024, USP will propose a new standard for digital verification - where the pharmacy’s system automatically cross-checks the strength against a national database. The goal? Zero preventable errors. The path? One step at a time. Verifying strength. Verifying quantity. Verifying the device. Every time.It’s Not Just a Procedure - It’s a Promise
Medication isn’t just a pill or a liquid. It’s trust. You trust the pharmacy to get it right. You trust the system to catch mistakes. But trust isn’t enough. You need verification. You need two eyes, two brains, and the right tools. Because when it comes to medication strength and quantity, there’s no room for “I thought.”Why is it dangerous to confuse strength per mL with total amount in the bottle?
Confusing strength per mL (like 10 mg/mL) with the total amount (like 30 mL) means you think the bottle has 10 mg of drug - when it actually has 300 mg. That’s a 30-fold overdose. This mistake has caused fatal reactions with insulin, opioids, and other high-alert medications. The FDA has documented multiple cases where patients received lethal doses because they - and even providers - misread the label.
Can I rely on the pharmacist to double-check my medication?
You should expect them to, but you can’t assume they always do. Many pharmacies, especially small or understaffed ones, face pressure to move prescriptions quickly. A 2023 survey found 73% of pharmacy techs felt rushed during verification. Always verify yourself - ask for the total amount, confirm the dosing device, and do the math. Your safety isn’t someone else’s job alone.
Why do pharmacies still give out teaspoons instead of syringes?
It’s outdated practice. Teaspoons vary in size - from 3 mL to 7 mL - and most people don’t measure accurately. The FDA and ISMP have banned this for pediatric meds since 2018. But some pharmacies still use them because they’re cheaper or patients ask for them. Always request an oral syringe, especially for doses under 10 mL. It’s safer, more precise, and required by best practice guidelines.
What should I look for on a medication label to avoid errors?
Look for two things: the strength per unit (e.g., 5 mg/mL) and the total volume (e.g., 15 mL). The total amount should be clearly labeled and in a larger font than the concentration. Avoid labels that only show concentration. Also check for leading zeros (0.5 mg, not .5 mg) and no trailing zeros (5.0 mg is wrong - it should be 5 mg). These formatting rules prevent decimal errors that cause tenfold overdoses.
Are there legal requirements for double-checking medication?
Yes. The Joint Commission requires it in hospitals. The DEA requires it for controlled substances like opioids and stimulants - pharmacists must initial verification logs. The FDA and USP have labeling rules that make it impossible to misread strength without violating standards. And under Medicare Part D, pharmacies must prove they have strength verification protocols to stay in network. This isn’t optional - it’s enforced.
What’s the most common mistake patients make with liquid meds?
Using household spoons. A teaspoon isn’t 5 mL - it’s often 4 or 6 mL. Parents think they’re giving the right dose, but they’re not. Studies show 93% of pediatric dosing errors come from spoon confusion. Always use the syringe or cup the pharmacy provides. If they don’t give one, ask for it. It’s your right.

paul walker
January 29, 2026 AT 00:34Man I never thought about how a teaspoon could be deadly. My mom used to use one for my asthma meds and I never questioned it. Thanks for the wake-up call.
Kacey Yates
January 30, 2026 AT 22:46As a nurse I’ve seen this too many times. Pharmacies still hand out spoons like they’re free candy. If you’re not asking for a syringe, you’re gambling with your kid’s liver. Stop being polite and demand the right tool.
Keith Oliver
January 31, 2026 AT 07:06Let’s be real - this isn’t about ‘double-checking.’ It’s about systemic negligence masked as ‘efficiency.’ The FDA’s guidelines are toothless without enforcement, and corporate pharmacies prioritize throughput over human life. You think a $0.85 syringe is expensive? Try paying for a pediatric ICU stay because some tech was rushing to hit their 35-scripts-per-hour quota. This isn’t a mistake - it’s a crime waiting to happen, and nobody’s getting fired for it.
Frank Declemij
February 1, 2026 AT 19:05Valid point about the math. Always multiply concentration by volume. 10 mg/mL times 30 mL is 300 mg. If the script says 50 mg, something is wrong. Simple arithmetic saves lives. No excuse for skipping it. Always verify. Always.
Pawan Kumar
February 2, 2026 AT 00:00Do you realize the pharmaceutical-industrial complex profits from these errors? They know parents won’t question labels. They know small pharmacies can’t afford barcode scanners. They know the system is rigged to fail. The FDA’s new rules? PR spin. The real solution? Nationalize pharmacies. No profit motive. No corner-cutting. Just safety. Wake up.
kabir das
February 2, 2026 AT 07:11Oh my GOD. I just remembered - my cousin’s baby almost died because of this. I’ve been having nightmares since. I went back to that pharmacy and screamed at the pharmacist. They said ‘it was an honest mistake.’ An honest mistake? That’s not a mistake - that’s negligence with a paycheck. I still can’t sleep. Please, if you’re reading this - don’t trust anyone. Do the math. Bring your own syringe. I’m not joking.
ryan Sifontes
February 2, 2026 AT 18:19Yeah ok. But how many people actually do this? Like, really? I’ve never seen anyone at the pharmacy do the math. Everyone just takes the bottle and leaves. This feels like one of those ‘you should’ things that nobody actually does.
Laura Arnal
February 3, 2026 AT 13:08Thank you for sharing this!! 🙏 I’m a mom of two and I always ask for the syringe now - even if they give me side-eye. I’ve even printed out the ISMP guidelines and handed them to pharmacists. One told me I was ‘too intense’ 😅 But my kids are alive, so I don’t care. You’re not being difficult - you’re being a superhero. 💪❤️