Drug Interactions with Specific Statins: Class Effects and Differences
Statin Interaction Checker
Result will appear here after checking
When you take a statin to lower your cholesterol, you’re not just managing one thing-you’re managing a web of possible drug interactions that can turn a safe treatment into a dangerous one. Not all statins are the same. Some are like fragile glass, easily shattered by common medications. Others are built tougher, with fewer pathways for trouble. Knowing the difference isn’t just helpful-it can save your muscles, your liver, and maybe your life.
Why Statin Interactions Matter More Than You Think
About 32 million Americans take statins. That’s one in five adults. And nearly half of them are also on at least one other medication-blood pressure pills, diabetes drugs, antibiotics, even over-the-counter supplements. That’s where things get risky. Statins work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. But how your body processes each statin varies wildly. Some are broken down by liver enzymes that other drugs also use. When two drugs compete for the same enzyme, one can pile up to toxic levels. That’s how a simple combo like simvastatin and clarithromycin can spike statin levels by 10 times and trigger muscle breakdown-rhabdomyolysis-a rare but deadly condition that can lead to kidney failure.Metabolism Matters: CYP Enzymes and the Statin Divide
The biggest split among statins comes down to how they’re processed. Five of the seven main statins-atorvastatin, simvastatin, lovastatin, fluvastatin, and the now-withdrawn cerivastatin-rely on cytochrome P450 enzymes, especially CYP3A4 and CYP2C9. The other three-pravastatin, rosuvastatin, and pitavastatin-barely use these enzymes at all.- Simvastatin, lovastatin, and atorvastatin are mostly handled by CYP3A4. That means anything that blocks this enzyme-like the antibiotic clarithromycin, the antifungal ketoconazole, or HIV drugs like ritonavir-can cause a dangerous backup. Clarithromycin can make simvastatin levels jump 10-fold. For lovastatin? Up to 16-fold.
- Fluvastatin leans on CYP2C9, so it’s more at risk from drugs like warfarin or the diabetes medication glimepiride.
- Pravastatin, rosuvastatin, and pitavastatin are mostly cleared by the kidneys or through glucuronidation. They don’t rely heavily on CYP enzymes, so they’re far less likely to clash with common antibiotics or antivirals.
This isn’t just theory. A 2016 American Heart Association review found that patients on simvastatin and clarithromycin had a 3.5 times higher risk of hospitalization for muscle injury than those on pravastatin with the same antibiotic.
OATP1B1: The Hidden Player in Statin Safety
There’s another system at work: the OATP1B1 transporter. This protein shuttles statins into liver cells where they’re supposed to work. If something blocks it, the statin stays in your blood instead-raising your risk of side effects. Drugs like cyclosporine (used after transplants), gemfibrozil (a fibrate for triglycerides), and even some HIV meds can jam this transporter. The result? Rosuvastatin levels can rise by 7.1-fold with cyclosporine. Pitavastatin? Same thing. Pravastatin? Only a 1.5-fold increase. That’s why the FDA explicitly says: don’t combine cyclosporine with lovastatin, simvastatin, or pitavastatin. But pravastatin? It’s okay up to 40 mg daily.Even something as common as colchicine-used for gout flares-can raise statin levels slightly. Your doctor might not cut your statin, but they’ll watch you closer for muscle pain or weakness.
Which Statin Is Safest With Other Meds?
Here’s the real-world breakdown:| Statin | Primary Metabolism | High-Risk Drug Examples | Interaction Severity | Safer Alternatives |
|---|---|---|---|---|
| Simvastatin | CYP3A4 | Clarithromycin, diltiazem, cyclosporine, grapefruit juice | Very High | Pravastatin, rosuvastatin |
| Lovastatin | CYP3A4 | Clarithromycin, HIV protease inhibitors, grapefruit juice | Very High | Pravastatin, rosuvastatin |
| Atorvastatin | CYP3A4 | Clarithromycin, cyclosporine, diltiazem | Moderate to High | Pravastatin, rosuvastatin |
| Fluvastatin | CYP2C9 | Warfarin, fluconazole, glimepiride | Moderate | Pravastatin, rosuvastatin |
| Pravastatin | Renal (minimal CYP) | Cyclosporine (low risk), gemfibrozil | Lowest | - |
| Rosuvastatin | Minimal CYP, OATP1B1 | Cyclosporine, gemfibrozil | Moderate (OATP1B1 only) | Pravastatin |
| Pitavastatin | Glucuronidation, OATP1B1 | Cyclosporine, gemfibrozil | High (OATP1B1) | Pravastatin |
Pravastatin stands out. It’s not metabolized by CYP enzymes. It doesn’t rely on liver transporters the same way. It’s excreted mostly through the kidneys. That makes it the safest bet for patients on multiple meds-especially those with HIV, heart transplants, or chronic kidney disease.
When Fibrates and Statins Mix
Fibrates like gemfibrozil and fenofibrate are often paired with statins to tackle both cholesterol and triglycerides. But gemfibrozil is a troublemaker. It blocks not just CYP2C8 but also glucuronidation-the backup cleanup system for statins. That’s why it can double statin levels and make muscle damage far more likely.The American College of Cardiology says: avoid gemfibrozil with any statin except pravastatin. If you need a fibrate, choose fenofibrate instead. It doesn’t interfere with statin metabolism the same way. It’s a safer combo.
What About Ticagrelor and Other Heart Drugs?
Ticagrelor (Brilinta) is a blood thinner used after heart attacks or stents. It’s often prescribed with statins. But here’s the catch: ticagrelor can slightly raise atorvastatin levels. Not enough to be dangerous. The 2022 ACC guidelines say you can still use atorvastatin with ticagrelor-just avoid high doses of simvastatin or lovastatin. Stick to 40 mg or less if you’re on those.Calcium channel blockers like diltiazem and verapamil? They’re common for high blood pressure. But they also block CYP3A4. If you’re on simvastatin or lovastatin, your doctor might switch you to pravastatin or rosuvastatin-or lower your statin dose.
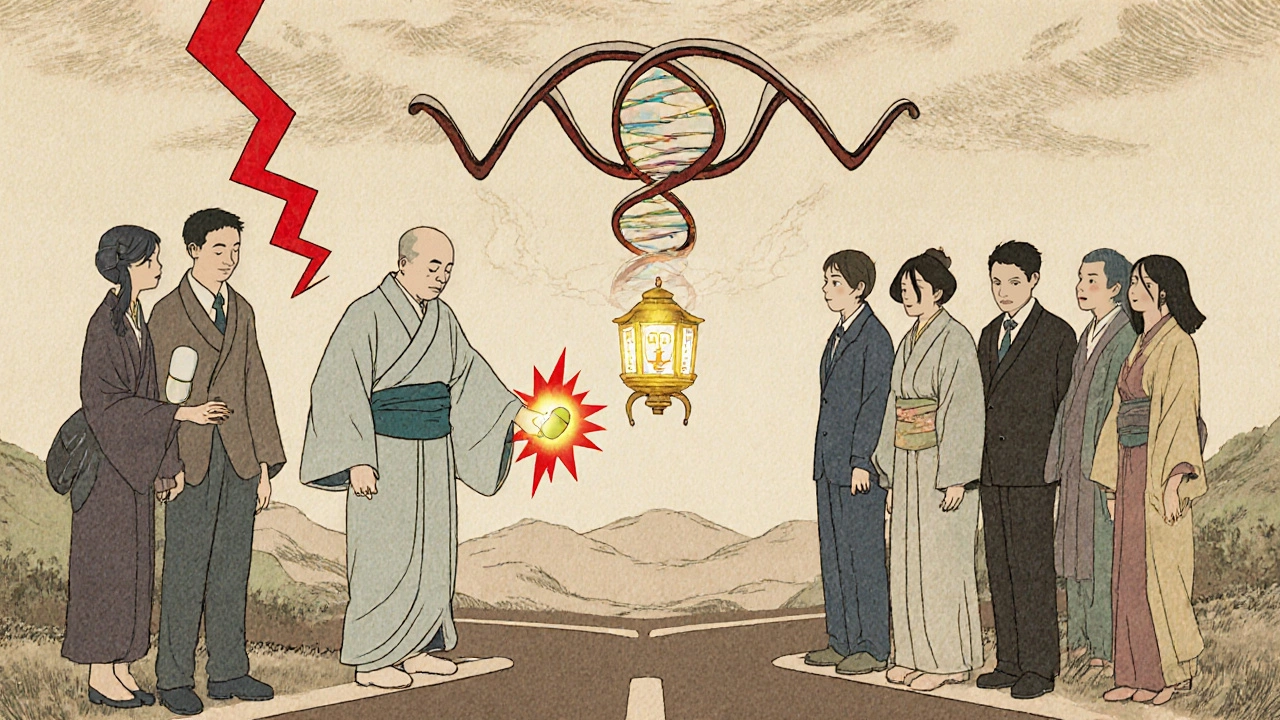
Genetics Play a Role Too
Your genes matter. A common variation in the SLCO1B1 gene-called the c.521T>C polymorphism-makes some people absorb statins too well. This single gene change can raise the risk of muscle damage from simvastatin by 4.5 times. It’s why some people get muscle pain on a low dose while others take 80 mg with no issues.The FDA added this genetic info to simvastatin’s label back in 2011. But most doctors don’t test for it-yet. If you’ve had unexplained muscle pain on a statin, especially simvastatin, ask if genetic testing might help. It’s not routine, but it could explain why one drug didn’t work for you while another did.
What You Should Do
- If you’re on multiple medications, ask your doctor which statin is safest for you-not just which one lowers cholesterol the most.
- Never start a new prescription, supplement, or OTC drug without checking for statin interactions. Even St. John’s wort or red yeast rice can interfere.
- If you feel unexplained muscle pain, weakness, or dark urine, stop the statin and call your doctor immediately. Don’t wait.
- Pravastatin is often the best choice if you’re on HIV meds, immunosuppressants, or multiple heart drugs.
- Avoid simvastatin 80 mg entirely. The FDA warns it offers no extra heart benefit but doubles the risk of muscle damage.
What’s Next?
New drugs like bempedoic acid (Nexletol) are coming onto the scene. They lower LDL without relying on the same liver pathways as statins-and they have almost no drug interactions. In the CLEAR Outcomes trial, it cut heart attacks and strokes by 17% with minimal interaction risk.Meanwhile, researchers are building tools that use your genetic data, current meds, and liver function to predict your statin risk before you even start. These systems could soon tell your doctor: “Don’t give simvastatin to this patient. Give pravastatin instead.”
For now, the message is simple: statins save lives. But not all statins are equal. The right one for you depends on what else you’re taking. Don’t assume your statin is safe just because your doctor prescribed it. Ask the question. Know the difference. Your muscles-and your heart-will thank you.
Can I drink grapefruit juice with my statin?
No, not if you’re taking simvastatin, lovastatin, or atorvastatin. Grapefruit juice blocks CYP3A4, the same enzyme that breaks down these statins. One glass can raise their levels by up to 15 times, increasing your risk of muscle damage. Pravastatin, rosuvastatin, and pitavastatin are safer options if you want to keep drinking grapefruit juice-but even then, moderation is best.
Is pravastatin the safest statin overall?
For people taking multiple medications-especially HIV drugs, transplant meds, or antibiotics-yes. Pravastatin doesn’t rely on CYP enzymes and has the lowest interaction risk of any statin. It’s also the only one the FDA says is safe to take with cyclosporine at standard doses. That makes it the go-to choice for complex medication regimens.
Why is simvastatin 80 mg no longer recommended?
The FDA and American Heart Association pulled the 80 mg dose of simvastatin because studies showed it didn’t offer more heart protection than lower doses-but it doubled the risk of rhabdomyolysis. The risk is highest in the first year, especially in older adults or those with kidney problems. Stick to 20-40 mg unless your doctor has a very specific reason to go higher.
Can I take statins with antibiotics?
It depends. Antibiotics like clarithromycin and erythromycin are dangerous with simvastatin, lovastatin, and atorvastatin. Azithromycin is safe. Amoxicillin and ciprofloxacin don’t interfere. Always tell your pharmacist or doctor what statin you’re on before starting any new antibiotic. Never assume it’s safe.
What should I do if I start feeling muscle pain?
Stop the statin and call your doctor right away. Muscle pain, weakness, or dark urine could be signs of rhabdomyolysis. Your doctor will check your creatine kinase (CK) levels and may switch you to a safer statin like pravastatin or rosuvastatin. Don’t wait for symptoms to get worse. Early action prevents serious damage.

Will Phillips
November 19, 2025 AT 22:44Statins are just another way the pharmaceutical industry keeps us hooked. They don't cure anything they just make you dependent. And don't get me started on grapefruit juice being banned with statins. That's a corporate lie to push more pills. My uncle took simvastatin for 12 years and never had a problem. They're just scared of natural alternatives.
Arun Mohan
November 20, 2025 AT 20:12Pravastatin? How quaint. In my clinic in Delhi, we use rosuvastatin for 90% of cases. The pharmacokinetics are far superior, and the cost differential is negligible when you factor in reduced monitoring. The CYP3A4 narrative is outdated. OATP1B1 polymorphisms are the real frontier. Also, why are we still talking about grapefruit juice? It's 2025. We have pharmacogenomic panels now.
Tyrone Luton
November 21, 2025 AT 17:46There's a deeper truth here. Statins aren't about cholesterol. They're about control. The body makes cholesterol because it needs it. The liver isn't broken. It's being overruled. We've turned a natural process into a criminal act. And now we're told to avoid grapefruit because it 'interferes'-as if nature itself is the enemy. What if the real problem isn't the statin, but the belief that we can engineer our way out of biology with chemistry?
Jeff Moeller
November 22, 2025 AT 00:01Pravastatin is the quiet hero. No drama. No enzyme wars. Just kidneys doing their job. Simvastatin is like a firecracker in a library. One wrong move and everything blows up. The real takeaway? Don't overcomplicate it. If you're on five meds, pick the one that doesn't need a PhD to manage. Simple wins.
Herbert Scheffknecht
November 23, 2025 AT 10:23Let's not pretend this is science. This is a corporate taxonomy dressed up as medical guidance. Who decided that CYP3A4 was the villain? Who funded the studies that made simvastatin 80mg 'unsafe'? And why does every guideline suddenly love pravastatin after the patent expired? The FDA doesn't care about your muscles. They care about liability. The genetic testing? That's a profit center for labs. Your doctor won't test you because it costs $300 and insurance won't pay. So we're left with guesswork. And guess what? We're all just lab rats in a drug company's spreadsheet.
Jessica Engelhardt
November 24, 2025 AT 08:28Oh please. Pravastatin is the safest? Sure, if you're okay with it being half as effective. And don't get me started on 'gemfibrozil is bad'-that's just Big Pharma pushing rosuvastatin. We used to use fenofibrate in the 90s and nobody died. Now every doc wants the most expensive option because they're paid to. And don't even mention the 80mg simvastatin ban. That was a lawsuit waiting to happen. Not science. Just fear.
Martin Rodrigue
November 25, 2025 AT 15:17While the article presents a comprehensive overview of statin pharmacokinetics, it is regrettable that the discussion of OATP1B1 polymorphisms remains superficial. The c.521T>C variant demonstrates a dose-dependent effect on plasma concentrations, particularly with simvastatin, and should be integrated into pre-prescription screening protocols. Furthermore, the omission of recent data from the 2023 EAS Consensus on statin selection in polypharmacy is notable. A more rigorous approach would reference the GRADE methodology applied in the 2022 meta-analysis by Tanaka et al.
Sherri Naslund
November 27, 2025 AT 00:53ok so i read this and im like wow but wait… what if the whole cholesterol thing is a scam? like… what if heart disease is actually caused by sugar and stress and statins are just a distraction? my cousin took them for 3 years and got cancer. coincidence? maybe. but why dont they talk about that? also i heard grapefruit juice cures cancer so why are we scared of it??
Ashley Miller
November 27, 2025 AT 14:18Of course they say pravastatin is safe. It's the one they can't patent. Meanwhile, the real danger is the blood pressure meds they give you after you're on statins. They're all linked to the same CYP system. It's a trap. You start with one pill, then you need two, then three. Soon you're on a cocktail they designed to keep you buying. And don't even get me started on the 'FDA says' nonsense. That agency is owned by Big Pharma. Wake up.
Lauren Hale
November 29, 2025 AT 05:19If you're taking multiple medications, this is the kind of info you need to ask your pharmacist about-not just your doctor. I work in a community pharmacy and I see people on simvastatin with clarithromycin all the time. They have no idea. The safest thing you can do is make a list of everything you take-prescriptions, supplements, even herbal teas-and bring it to your pharmacist. They'll flag the bad combos. No judgment. Just help. Pravastatin really is the quiet winner for complex cases. And yes, grapefruit juice is a no-go with most statins. But if you love it, switch to rosuvastatin. It's not that hard.
Greg Knight
November 30, 2025 AT 18:59Look, I get it. This stuff is overwhelming. You're trying to stay healthy and now you're drowning in enzyme pathways and transporter proteins. But here's the good news-you don't need to be a scientist. You just need to be smart. Ask your doctor: 'What's the safest statin for me, given what else I'm taking?' Write it down. Then ask your pharmacist: 'Is this combo okay?' They're trained for this. And if you feel muscle pain, don't ignore it. That's your body screaming. Stop the med. Call your doctor. Don't wait. You're not being paranoid-you're being responsible. And if pravastatin works for you? That's not boring. That's winning.
rachna jafri
December 1, 2025 AT 16:29They call it medicine but it's just control. Statins are a tool to keep the poor docile while the rich get gene therapies. Why do you think they banned simvastatin 80mg? Because rich people don't take it-they get the new fancy ones. And grapefruit? That's a symbol. The system tells you what to eat, what to avoid, what to fear. But in India, we've been drinking lime juice with our meds for centuries. No one died. They just want you to trust them. Don't. Question everything. Your body knows more than any algorithm. And if you're on ten pills? Maybe you don't need any. Maybe you need food. Maybe you need rest. Maybe you need to stop being afraid. Statins are not the answer. The answer is asking why you need them in the first place.