Estrogen Deficiency: Why It Causes Dryness and Itching

Estrogen Deficiency Treatment Advisor
How This Tool Works
Answer a few questions about your symptoms and health history, and we'll help you identify which treatment options might be most suitable for you. This tool is for informational purposes only and shouldn't replace medical advice from a healthcare professional.
Assess Your Symptoms
Personalized Recommendations
Your ProfileRecommended Options
Based on your responses, we recommend considering these treatment options.
Hormone Replacement Therapy (HRT)
Best for moderate to severe symptoms with no contraindications. Provides comprehensive relief over 2-4 weeks but requires medical supervision due to potential risks.
Vaginal Moisturizers
Ideal for mild to moderate symptoms. Provides hydration every 2-3 days and is non-systemic with minimal side effects.
Considerations
Key FactorsIf you’ve ever wondered why a drop in hormones brings on uncomfortable dryness and relentless itching, you’re not alone. estrogen deficiency is the hidden culprit behind many of these symptoms, especially during menopause or after certain medical procedures. Below we break down the science, the signs to watch for, and the steps you can take to find relief.
What is Estrogen Deficiency?
Estrogen deficiency is a condition where the body produces insufficient estrogen, a hormone that plays a crucial role in regulating numerous bodily functions. It commonly occurs during menopause, the natural transition marking the end of menstrual cycles, but can also follow surgical removal of the ovaries, certain cancer treatments, or chronic health issues.
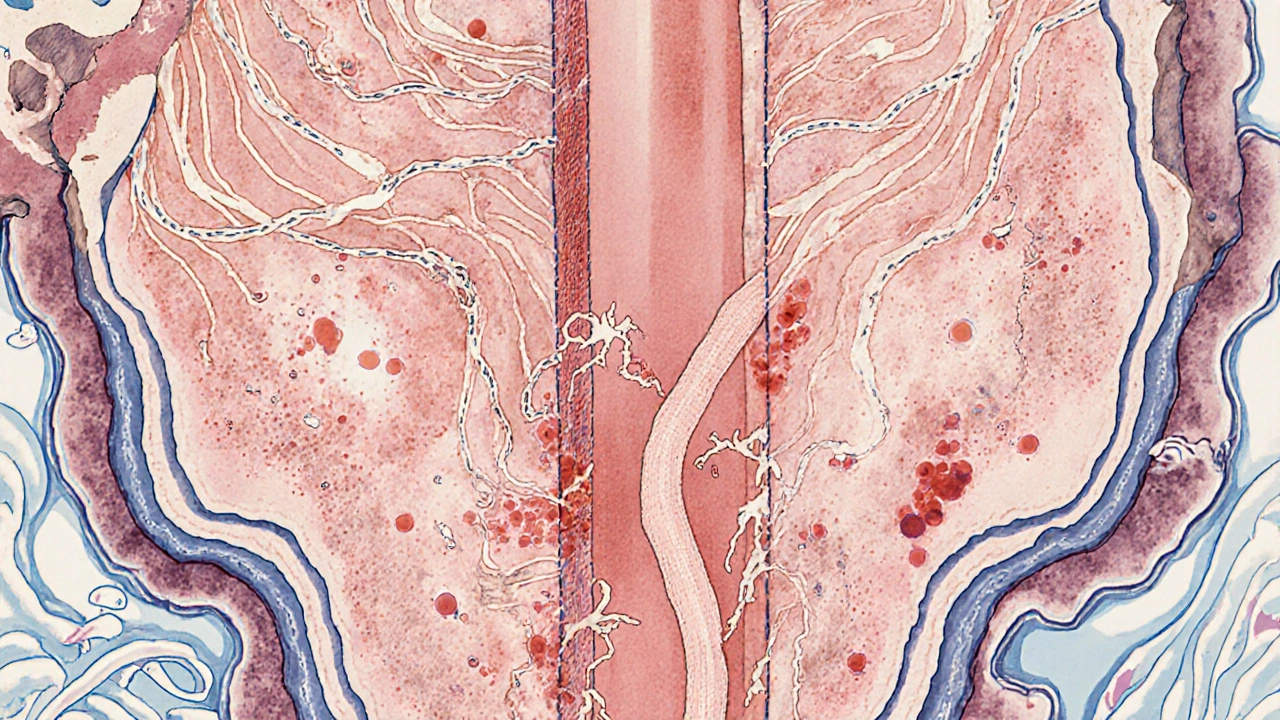
Estrogen’s Role in Maintaining Moisture and Skin Barrier
Estrogen isn’t just a reproductive hormone; it actively supports the health of epithelial tissues, including the lining of the vagina and the surrounding skin. It stimulates the production of glycogen, a sugar that attracts water into the vaginal walls, and enhances blood flow, which together keep the tissue supple and well‑lubricated. Moreover, estrogen helps maintain the integrity of the skin barrier function by promoting collagen synthesis and preserving the natural lipid layer.
Why a Drop in Estrogen Leads to Dryness
When estrogen levels fall, several physiological changes occur:
- Reduced glycogen stores mean less water is retained in the mucosal cells, making the tissue feel thin and dry.
- Decreased blood flow limits the delivery of nutrients and moisture to the area.
- Collagen breakdown weakens tissue elasticity, allowing it to become fragile.
The combined effect is the classic symptom of vaginal dryness, which can range from mild discomfort during everyday activities to painful intercourse (dyspareunia).
Why Itching Often Follows Dryness
Dry tissue is more prone to irritation. As the protective mucus layer thins, tiny fissures appear in the epithelial surface. These micro‑tears expose nerve endings, triggering the sensation of itch. Additionally, a compromised barrier makes it easier for irritants-such as soaps, laundry detergents, or even normal bacterial flora-to provoke an inflammatory response.
Common Triggers and Risk Factors
Besides natural hormonal decline, several factors can worsen dryness and itching:
- Smoking - damages blood vessels and reduces estrogen synthesis.
- Chronic stress - elevates cortisol, which can suppress estrogen production.
- Certain medications - especially antihistamines and some antidepressants that have drying side effects.
- Excessive hygiene - aggressive cleansing strips away natural lubrication.
Identifying and modifying these contributors can significantly improve symptoms.
How Doctors Diagnose Estrogen‑Related Dryness
Diagnosis starts with a clinical interview and a pelvic exam. Physicians often assess:
- The appearance of the vaginal walls (pale, thin, and lacking rugae).
- pH level - a rise above 4.5 suggests reduced estrogen protection.
- Patient‑reported symptom severity using standardized scales.
When needed, a blood test measures blood estrogen level, typically expressed as estradiol (E2) concentration. Values below 30 pg/mL in post‑menopausal women often confirm deficiency.
Managing Dryness and Itching
Effective relief usually combines lifestyle tweaks, topical products, and, when appropriate, hormonal therapy. Below is a quick comparison of the most common options.
| Option | How It Works | Onset of Relief | Pros | Cons |
|---|---|---|---|---|
| Hormone Replacement Therapy (HRT) | Restores systemic estrogen levels, improving tissue health throughout the body. | 2-4 weeks | Comprehensive symptom relief; also benefits bone health. | Potential risk of blood clots, breast cancer; requires medical supervision. |
| Vaginal moisturizers | Provides long‑lasting hydration by forming a protective barrier. | Within days | Non‑systemic; easy to use; safe for most women. | May need frequent re‑application; less effective for severe atrophy. |
| Vaginal lubricants | Reduces friction during sexual activity. | Immediate | Perfect for occasional use; no hormones. | Short‑acting; does not treat underlying dryness. |
| Phytoestrogen‑rich foods or supplements | Plant‑derived compounds bind estrogen receptors mildly. | Weeks to months | Natural, low‑risk, may improve mild symptoms. | Variable potency; not a substitute for medical HRT in severe cases. |
When choosing a path, consider severity, personal health history, and comfort with hormonal interventions. Below are practical tips for each approach.
- HRT: Discuss dosage, delivery method (pill, patch, gel, or vaginal ring), and follow‑up labs with your provider.
- Moisturizers: Apply a pea‑sized amount every 2-3 days; look for products containing hyaluronic acid or vitaminE.
- Lubricants: Opt for water‑based, silicone‑free formulas if you have sensitivities.
- Phytoestrogens: Incorporate soy, flaxseed, or red clover into meals; consult a dietitian if you’re on blood‑thinners.

Preventive Lifestyle Practices
Even before symptoms appear, certain habits can keep estrogen‑related dryness at bay:
- Stay hydrated - aim for at least 8 glasses of water a day.
- Choose breathable cotton underwear; avoid tight synthetic fabrics.
- Limit douching and scented soaps; they disrupt natural pH.
- Engage in regular pelvic floor exercises (Kegels) to improve blood flow.
- Maintain a balanced diet rich in omega‑3 fatty acids, which support skin elasticity.
When to Seek Medical Help
If dryness interferes with daily life, causes persistent pain, or is accompanied by unusual discharge, it’s time to see a clinician. Red flag signs include:
- Sudden bleeding or spotting.
- Severe burning that doesn’t improve with moisturizers.
- Recurrent urinary tract infections.
- Any new lumps or masses.
Early evaluation can rule out infections, skin conditions, or, rarely, malignancy.
Frequently Asked Questions
Can estrogen deficiency cause skin dryness outside the vaginal area?
Yes. Estrogen helps maintain overall skin hydration by supporting collagen and natural oils. Low estrogen can lead to dry, itchy skin on the arms, legs, and face, especially after menopause.
Is over‑the‑counter (OTC) moisturizer enough for severe atrophy?
OTC moisturizers work well for mild to moderate symptoms, but severe atrophic changes often need systemic or local estrogen therapy for lasting improvement.
Are there risks associated with vaginal estrogen creams?
Vaginal estrogen delivers a low dose locally, minimizing systemic exposure. Risks are low but may include mild irritation or rare allergic reactions. Discuss any history of hormone‑sensitive cancers with your doctor.
Can lifestyle changes reverse estrogen deficiency?
Lifestyle can mitigate symptoms but cannot replace the hormone itself. Exercise, nutrition, and stress management support overall health, while medical therapy addresses the underlying deficiency.
How often should I have my estrogen levels checked?
If you start HRT, doctors usually test estradiol and progesterone every 3-6months during the first year, then annually if levels remain stable.
Understanding the link between estrogen deficiency and those nagging symptoms empowers you to take the right steps. Whether you opt for simple moisturizers, dietary tweaks, or a tailored hormone regimen, relief is within reach.

Joanna Mensch
October 17, 2025 AT 18:20They don't want you to know that the whole "estrogen deficiency" story is a convenient cash‑cow for Big Pharma, a covert operation to keep women dependent on pricey hormone pills while the real solution is hidden in plain sight, like diet and stress‑free living.
RJ Samuel
October 17, 2025 AT 19:26Honestly, the science is crystal clear: estrogen levels naturally dip during menopause, and the symptoms you describe are documented in countless peer‑reviewed studies, not some shadowy corporate plot.
Nickolas Mark Ewald
October 17, 2025 AT 21:40Great summary of the issue. For anyone dealing with dryness, keeping hydrated, using fragrance‑free moisturizers, and doing pelvic floor exercises can make a noticeable difference before jumping to prescriptions.
Chris Beck
October 17, 2025 AT 23:03Well UK women have been dealing with this forever while US media just sells you creams and pills!!!! The real problem is a broken healthcare system that pushes profit over care!!!
Emily Rankin
October 18, 2025 AT 01:50The intimate connection between our hormones and the very texture of our bodies reads like a quiet epic, a narrative where chemistry silently scripts our comfort. When estrogen whispers its presence, the skin and mucous membranes respond with a generous cascade of moisture and resilience. In the absence of that whisper, the landscape of the body changes, subtly at first, then with a plaintive ache that can feel almost existential. This transformation is not merely a physiological hiccup but a reminder of the fragile equilibrium we inhabit. It calls us to listen to the body’s language, to honor the signals that have been dismissed as "just aging." The dryness and itching become metaphors for the larger disconnection many feel from their own selves in modern life. By addressing the hormonal root, we are not just applying a cream; we are restoring a dialogue between mind, body, and the environment. Lifestyle choices-hydration, balanced nutrition, mindful stress reduction-act like supporting actors that reinforce the lead role of estrogen. Yet we must also recognize that for some, the deficit is too great for lifestyle alone, and medical intervention becomes an act of self‑compassion. The stigma surrounding hormone therapy often stems from fear, not from evidence, and it is our collective responsibility to demystify it. In the grand theater of health, every woman deserves a script that includes options, not a single‑track narrative. Embracing both natural and clinical remedies reflects a holistic philosophy that values science and personal agency alike. As we share stories of relief-whether from a simple moisturizer or a prescribed estrogen patch-we knit a community of support that transcends private discomfort. Let us celebrate the small victories, the moments when a once‑irritating itch fades, as they signal a reclaiming of bodily harmony. In doing so, we rewrite the tale of estrogen deficiency from one of helplessness into a testament of empowered healing.
Rebecca Mitchell
October 18, 2025 AT 02:06I love how you framed it honestly i think we all need a simple plan try a daily moisturizer and a glass of water
Roberta Makaravage
October 18, 2025 AT 02:40Estrogen isn’t a myth, it’s a hormone that actually exists 🌸💊
Lauren Sproule
October 18, 2025 AT 03:46Hey there! I totally get where you're coming from-sometimes the medical jargon can feel like a wall of confusing words. It’s okay to feel a little overwhelmed, but remember you’re not alone in this journey. A simple tip that helped many folks is to start with a gentle, fragrance‑free moisturizer; apply it after a warm shower when your skin is still a bit damp for best absorption. Also, drinking enough water throughout the day can make a big difference, even if it sounds basic. If you ever feel uncertain about trying a new product, chatting with a friendly pharmacist can give you peace of mind without the scare factor. And don’t forget the power of a good pelvic floor routine-just a few minutes a day can boost blood flow and improve comfort. You’ve got this, and every small step adds up to a big improvement over time. Keep listening to your body, and be kind to yourself as you explore what works best. If you need more ideas, just shout-there’s a whole community ready to share their tips and tricks. Stay hopeful, stay hydrated, and most importantly, stay you!
CHIRAG AGARWAL
October 18, 2025 AT 05:26This article is way too long and full of boring science – I could just skim the headings and be done.
genevieve gaudet
October 18, 2025 AT 06:33While brevity has its place, the depth here mirrors how many cultures treat the body as a story, not just a machine. In some traditions, the balance of hormones is linked to seasonal rituals and diet, so the detailed explanation actually resonates with a broader worldview. It invites us to see personal health as part of a larger cultural tapestry.