Hormone Therapy for Breast Cancer: Tamoxifen vs Aromatase Inhibitors Explained

What Is Hormone Therapy for Breast Cancer?
Not all breast cancers are the same. About 8 out of 10 breast cancers are hormone receptor-positive, meaning they grow in response to estrogen. Hormone therapy blocks this signal, starving the cancer cells of what they need to survive. It’s not chemotherapy. It doesn’t kill cells outright. Instead, it cuts off their fuel. For many women, this is the most important part of treatment after surgery or radiation.
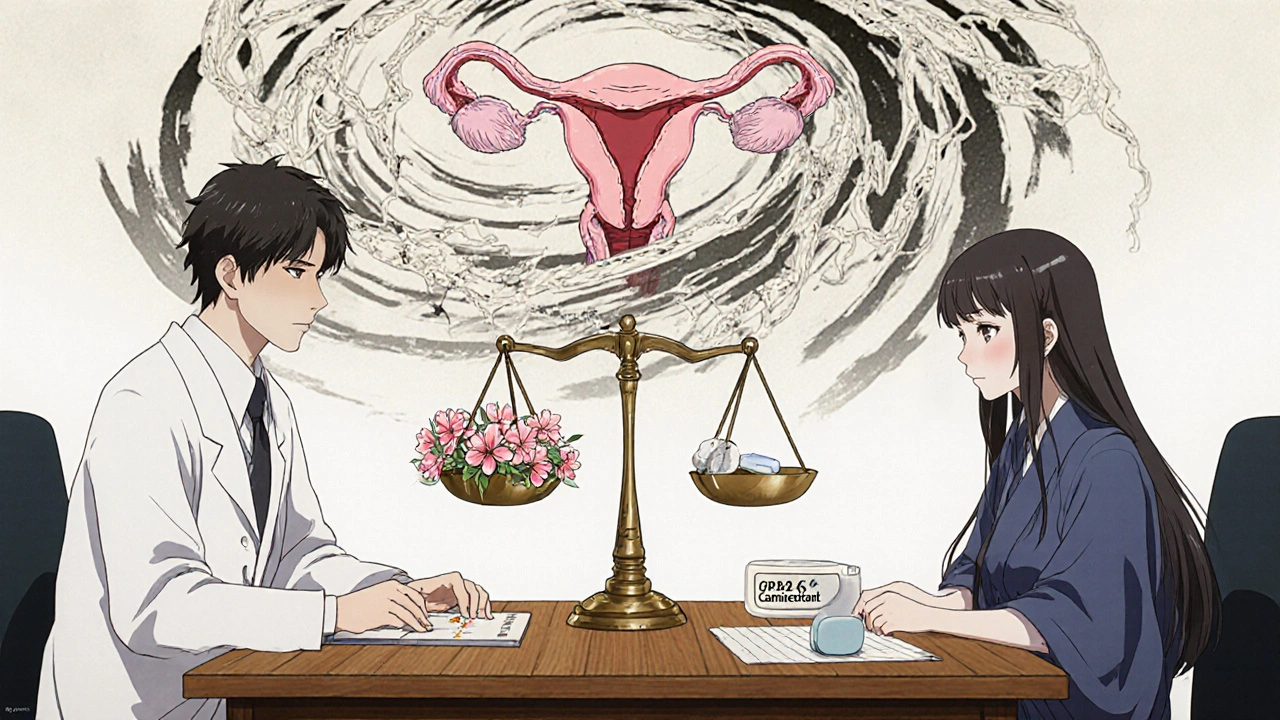
Two main types of hormone therapy dominate modern care: tamoxifen and aromatase inhibitors (AIs). Both work to lower estrogen’s effect on breast tissue, but they do it in completely different ways. Choosing between them isn’t about which is "better" overall-it’s about which fits your body, your life, and your risk level.
How Tamoxifen Works
Tamoxifen has been around since the 1970s. It’s a selective estrogen receptor modulator, or SERM. Think of it as a key that fits into estrogen’s lock on breast cancer cells-but instead of turning the lock open, it jams it. Estrogen can’t get in, so the cancer doesn’t get the signal to grow.
It’s taken as a daily pill, usually 20 mg. It stays active in your system for days after you stop taking it. That’s why you don’t need to time doses perfectly. What makes tamoxifen unique is that it acts differently in different parts of the body. In breast tissue, it blocks estrogen. In bone and the heart, it can act like estrogen, which is why it helps preserve bone density and may lower cholesterol.
But there’s a trade-off. In the uterus, tamoxifen can mimic estrogen too much. This raises the risk of endometrial cancer-about 1.2% over 10 years compared to 0.4% for women not on it. It also increases the chance of blood clots. About 0.76% of women on tamoxifen develop a pulmonary embolism, compared to 0.37% on AIs. These risks are higher in women over 50 or those who smoke.
How Aromatase Inhibitors Work
Aromatase inhibitors-like anastrozole (Arimidex), letrozole (Femara), and exemestane (Aromasin)-work by stopping estrogen production entirely. They target the aromatase enzyme, which turns male hormones (androgens) into estrogen in fat tissue, skin, and other places outside the ovaries.
After menopause, your ovaries stop making estrogen. But your body still makes small amounts through aromatase. AIs block this process by 95-98%. That’s why they’re only effective in postmenopausal women. If you’re still having periods, AIs won’t work unless you also suppress ovarian function with drugs like goserelin.
Unlike tamoxifen, AIs don’t help your bones or heart. In fact, they make them weaker. About 6.4% of women on AIs break a bone over 10 years, compared to 5.1% on tamoxifen. Joint pain is also common-up to half of women report moderate to severe aches, especially in hands, knees, and back. That’s why bone density scans (DEXA) are standard for anyone on AIs. If your T-score drops below -2.0, doctors often add drugs like denosumab or zoledronic acid to protect your bones.
Which One Is Better? It Depends on Your Menopausal Status
This is where things get personal. Your menopausal status determines which drug is right for you.
If you’re premenopausal, tamoxifen is the standard. AIs alone won’t work because your ovaries are still making estrogen. But if your cancer is higher risk, doctors may add ovarian suppression (OFS) with a monthly shot like goserelin. The TEXT and SOFT trials showed that when you combine exemestane with OFS, you cut recurrence risk by 21% compared to tamoxifen plus OFS. That’s one extra recurrence prevented for every 31 women treated this way.
If you’re postmenopausal, AIs are now the first choice. The ATAC trial showed that anastrozole reduced recurrence by 30% more than tamoxifen during treatment. Ten-year survival was better too: 12.1% of women on AIs died from breast cancer, compared to 14.2% on tamoxifen. That’s a real difference.
But here’s the catch: AIs work best in the first 4-5 years. After that, the gap closes. That’s why some women switch from tamoxifen to an AI after 2-3 years. Real-world data from the OBSERVATION registry shows this switch gives nearly the same results as starting with an AI.

Side Effects: What Women Actually Experience
Doctors talk about stats. Women talk about how they feel.
On forums like Breastcancer.org, 68% of AI users reported moderate to severe joint pain. About 22% stopped taking their meds because of it. For tamoxifen users, that number was 8%. On Reddit, women described "chemo brain" getting worse on AIs-trouble remembering names, losing track of conversations. Tamoxifen users mostly complained about hot flashes-63% said they were unbearable at first.
But AI users often feel relieved about one thing: no uterine cancer risk. Only 0.4% of women on AIs develop endometrial cancer, compared to 1.2% on tamoxifen. For women with a history of blood clots or who are overweight, that’s a major plus.
And then there’s bone health. One woman in Auckland, 67, started on letrozole after surgery. Her DEXA scan showed her bone density dropping fast. She started denosumab injections every six months. "I didn’t want to be the woman who broke a hip from a stumble," she said. "The shot hurts, but not as much as the fear."
How Long Do You Take It?
Five years is the standard. But for higher-risk cancers-larger tumors, spread to lymph nodes, high-grade tumors-doctors often recommend 7 to 10 years.
The MA.17X trial showed that extending AI therapy to 10 years reduced late recurrences. The DATA trial found similar benefits with extended tamoxifen. The key is matching length to risk. A woman with a small, low-grade tumor might do fine with 5 years. Someone with multiple positive lymph nodes might need 10.
Genomic tests like Oncotype DX help decide. If your Recurrence Score is below 25, you get almost no extra benefit from chemotherapy. That means hormone therapy alone is enough. You can focus on minimizing side effects instead of adding more drugs.
What About Cost and Access?
Tamoxifen costs about $15 a month as a generic. Brand-name AIs can run $150 a month. In the U.S., insurance usually covers them. But in low-income countries, tamoxifen is often the only option. In Japan, doctors still prefer tamoxifen for women under 70 because Asian populations have lower baseline fracture rates.
Even in wealthy places, cost matters. One woman in New Zealand switched from letrozole to tamoxifen after her insurance denied coverage. "I’d rather take the pill with more hot flashes than lose my home over a prescription," she said.
What’s Next? New Options on the Horizon
The field isn’t standing still. In 2023, the FDA approved camizestrant, a new oral SERD (selective estrogen receptor degrader). It doesn’t just block estrogen-it destroys the receptor itself. In the SERENA-2 trial, it cut recurrence by 38% compared to standard AI therapy in women with ESR1 mutations.
Another big question: Do you need 5 years of tamoxifen? The PERSEPHONE trial is testing whether 3 years is enough for low-risk patients. Early data suggests it might be.
And then there’s pharmacogenomics. About 7% of people are "poor metabolizers" of tamoxifen because of a CYP2D6 gene variant. Their bodies can’t turn tamoxifen into its active form, endoxifen. Studies show they have 2.5 times higher recurrence risk. Testing for this gene is still rare, but trials like CYRILLUS are pushing to make it standard.
Final Thoughts: It’s Not One Size Fits All
There’s no perfect drug. Tamoxifen protects your bones but risks your uterus. AIs protect your uterus but weaken your bones. Both cause fatigue. Both change your sex life. Both require years of commitment.
The best choice comes from knowing your cancer’s profile, your body’s response, and what matters most to you. Do you fear blood clots more than joint pain? Do you want to avoid surgery on your uterus? Are you willing to take a bone shot every six months to lower your recurrence risk by 3%?
That’s why doctors now talk about "shared decision-making." They give you the numbers. You tell them what you’re willing to live with. And together, you pick the path that fits your life-not just your diagnosis.
What to Ask Your Doctor
- Is my cancer hormone receptor-positive? What’s my ER/PR status?
- Am I pre- or postmenopausal? Do I need ovarian suppression?
- What’s my recurrence risk based on tumor size, grade, and lymph node status?
- Have I been tested for CYP2D6 gene variants if we’re considering tamoxifen?
- What’s my bone density? Do I need a DEXA scan before starting?
- What are the most common side effects I should prepare for?
- Can we start with one drug and switch later if needed?
- What happens if I can’t afford this medication?

Daisy L
November 22, 2025 AT 03:53Anne Nylander
November 23, 2025 AT 13:00i know it feels overwhelming but you’re not alone!!
so many women have been here and come out stronger!!
just take it one day at a time!!
you’re brave and you’re gonna beat this!! 💪❤️
Noah Fitzsimmons
November 25, 2025 AT 06:43Eliza Oakes
November 26, 2025 AT 22:02Swati Jain
November 27, 2025 AT 06:25jim cerqua
November 28, 2025 AT 06:43Erika Sta. Maria
November 30, 2025 AT 04:30we’re being sold drugs like they’re life coaches.
what if we just… ate more turmeric?
or meditated?
or stopped blaming our bodies for existing?
the real cancer is the system that makes us choose between bone density and uterine safety.
also i think the cyp2d6 test is bs because my cousin took tamoxifen and got pregnant. so… what does that even mean?
also why is everyone so scared of the uterus? it’s just a muscle.
🌿🧘♀️
Debanjan Banerjee
December 1, 2025 AT 23:57Elaina Cronin
December 2, 2025 AT 01:12Leo Tamisch
December 3, 2025 AT 18:24Corra Hathaway
December 4, 2025 AT 14:12Paula Jane Butterfield
December 6, 2025 AT 06:03Simone Wood
December 7, 2025 AT 00:17