How Comorbidities Increase Drug Side Effects: What You Need to Know
When you take a medication, you expect it to help - not hurt. But if you have one or more chronic health conditions, the risk of harmful side effects doesn’t just go up a little. It skyrockets. A study of over 1,100 patients found that nearly 20% of those with multiple health problems had an adverse drug reaction, compared to less than 8% of people with no other conditions. That’s more than double the risk. And it’s not because the drugs are weak or poorly made. It’s because your body doesn’t process them the same way anymore.
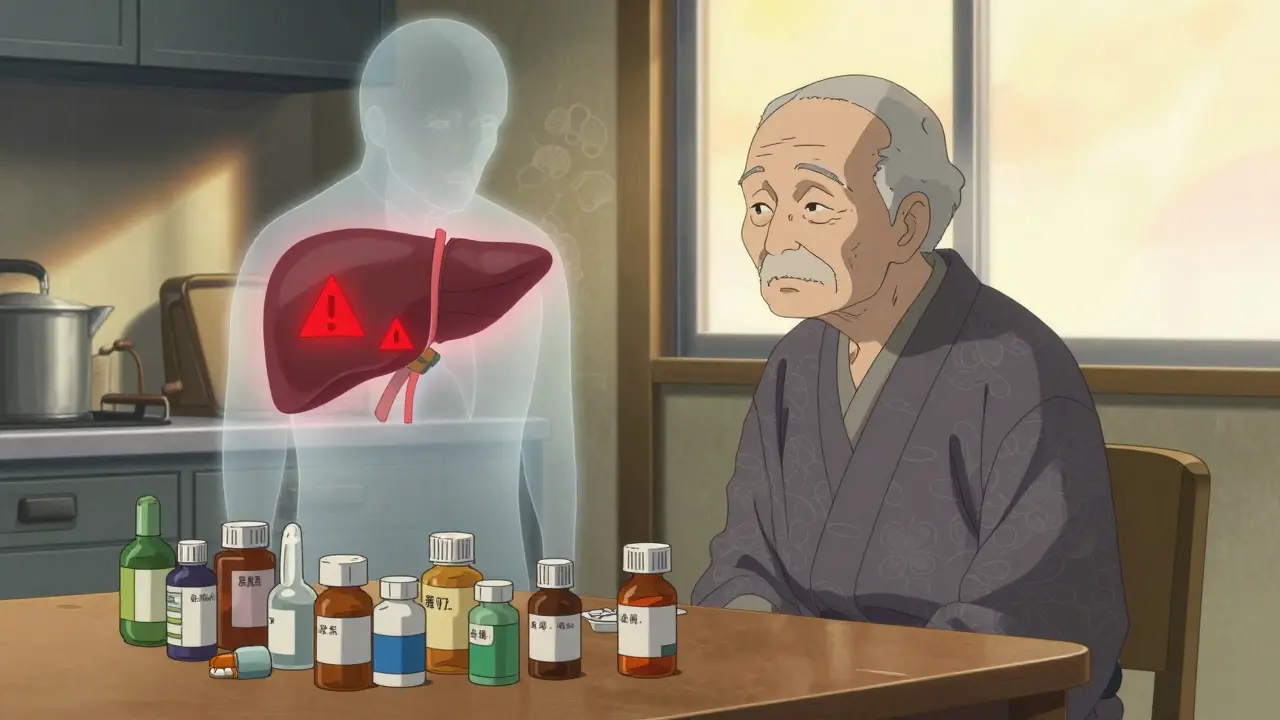
Why Your Other Health Conditions Change How Drugs Work
Your liver, kidneys, heart, and nervous system don’t just sit around while you take medicine. They’re actively involved in how drugs move through your body - where they go, how long they last, and how strongly they affect you. When you have conditions like diabetes, kidney disease, liver cirrhosis, or heart failure, these systems don’t work the way they used to. That changes everything.For example, if your liver is damaged from years of alcohol use or fatty liver disease, it can’t break down drugs as quickly. This means medications like painkillers, antidepressants, or even antibiotics stay in your bloodstream longer than they should. The result? Higher doses than intended, leading to dizziness, confusion, or even falls. One study showed liver disease cuts the activity of key drug-processing enzymes by 30% to 50%. That’s not a small tweak - it’s a major shift in how your body handles medicine.
Same goes for your kidneys. If your glomerular filtration rate (GFR) drops below 60 mL/min - a common sign of chronic kidney disease - drugs that are cleared through urine build up in your system. Blood pressure meds, diuretics, and even some antibiotics become more potent, increasing the chance of low blood pressure, electrolyte imbalances, or acute kidney injury.
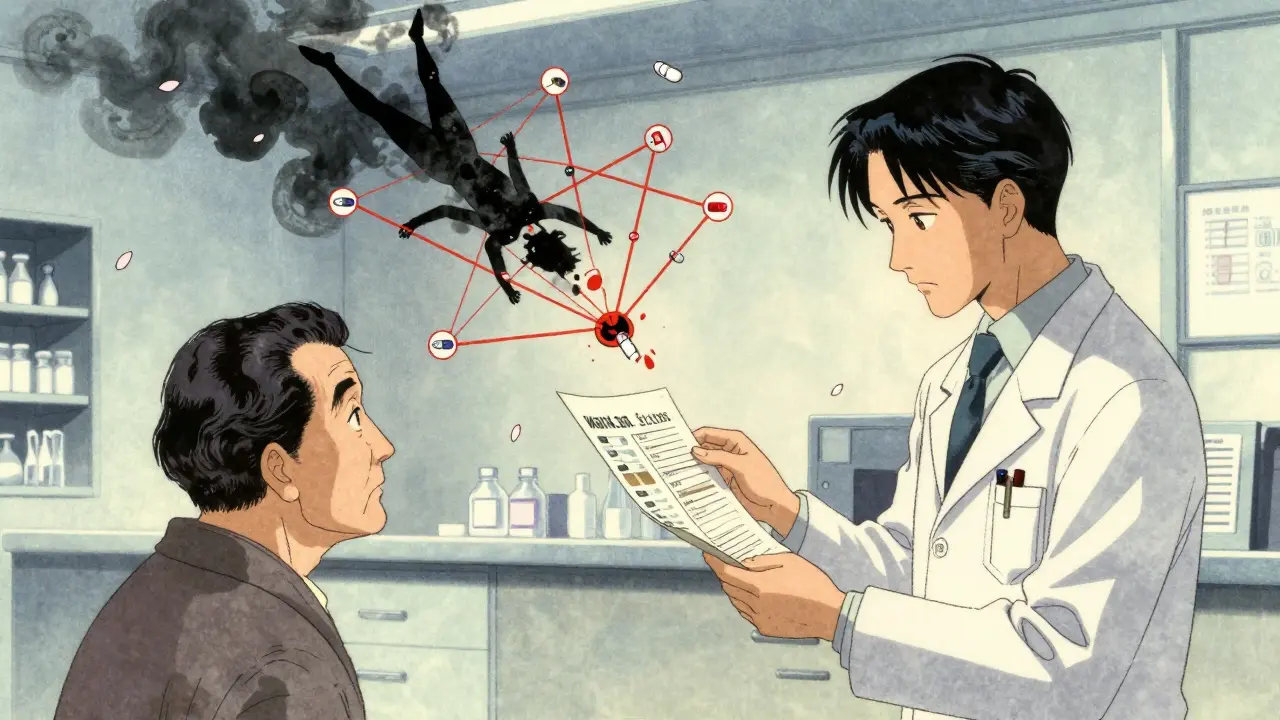
The Perfect Storm: Polypharmacy and Comorbidities
Most people with multiple health conditions don’t take just one or two pills. They take five, six, or even ten. In fact, nearly half of adults over 65 with two or more chronic diseases are on five or more medications daily. This isn’t just inconvenient - it’s dangerous.When you take multiple drugs at once, they can interact with each other in ways no doctor could predict without detailed tools. One study of 100 cancer patients found 65 drug-drug interactions - and over a third of those were serious enough to cause permanent harm or death. Even more alarming: 47% of elderly patients on multiple medications had at least one interaction that could lead to hospitalization.
These aren’t rare cases. In primary care clinics, 40% to 60% of medication problems in older patients come from these overlapping prescriptions. Anticoagulants, antihypertensives, and psychiatric drugs are the top three culprits. Warfarin, for example, becomes riskier if you also have kidney disease or take antibiotics that interfere with its metabolism. A simple change in one drug can send your INR levels spiraling - leading to internal bleeding.
What the Side Effects Look Like in Real Life
The side effects you get when you have comorbidities aren’t the same as those seen in healthy volunteers in drug trials. You’re not likely to just feel a little nauseous. You’re more likely to feel weak, dizzy, or confused - symptoms that can lead to falls, hospital stays, or even permanent disability.One large study tracked over 700 adverse drug reactions and found the most common symptoms in patients with multiple conditions were:
- Weakness - 36% of cases
- Dizziness - 11.8%
- Headache - 7.3%
- Nausea and vomiting - combined nearly 9%
- Insomnia - 2.9%
Notice something? Dizziness was a bigger problem in people without comorbidities - but in those with multiple conditions, weakness took the lead. That’s because their bodies can’t compensate. Their muscles are weaker, their balance is poorer, and their nervous systems are more sensitive. A drug that causes mild dizziness in a healthy person might knock someone with heart failure and arthritis off their feet.
Who’s at Highest Risk - And Why
It’s not just about how many conditions you have. It’s about which ones. Certain combinations are especially dangerous.Patients with substance use disorders are 77% to 93% more likely to also smoke. That means they’re taking medications while their liver is already under stress from nicotine and alcohol - making them far more vulnerable to liver toxicity from drugs like acetaminophen or statins.
Chronic pain patients are another high-risk group. About 10% misuse their opioid prescriptions, and that misuse often leads to respiratory depression, addiction, or overdose - especially when combined with benzodiazepines or sleep aids. The FDA now requires warnings on these combinations because they’ve caused thousands of preventable deaths.
And then there’s age. Older adults are disproportionately affected. Nearly half of seniors over 65 are prescribed at least one medication listed in the Beers Criteria - drugs that are known to be risky for older people. Women over 75 are nearly three times more likely to be prescribed these dangerous drugs than younger women. Why? Because doctors often don’t realize how much aging changes drug metabolism - or they’re pressured to treat every symptom with a pill.
The Hidden Gap: Why Clinical Trials Don’t Tell the Whole Story
Most drug trials exclude people with multiple chronic conditions. They want clean data - so they pick healthy volunteers or patients with just one disease. But in real life, that’s not who needs the medicine.Up to 80% of elderly patients with three or more conditions were left out of the studies that approved the drugs they’re now taking. That means we don’t know how those drugs really behave in people with kidney disease, dementia, and heart failure all at once. We’re guessing. And sometimes, that guess kills.
This is why the FDA now requires new drug applications to include subgroup analyses for patients with common comorbidities - up from 42% in 2018 to 78% in 2023. It’s progress. But it’s still not enough.
What Can Be Done? Practical Steps to Reduce Risk
You don’t have to accept high risk as normal. There are proven ways to cut down on dangerous side effects.Get a medication review. A clinical pharmacist can go through every pill, patch, and supplement you take - and spot interactions your doctor might miss. One study showed this reduced adverse reactions by 22% in just six months.
Ask about deprescribing. Not every medication you’ve been on for years is still necessary. The STOPP/START guidelines help doctors decide what to stop and what to keep. Patients who followed these protocols had 17% fewer hospital visits due to drug reactions.
Use technology. Electronic health records with built-in comorbidity alerts can flag risky combinations before a prescription is written. Hospitals using these systems saw a 35% drop in inappropriate prescribing for patients with kidney or liver disease.
Track your symptoms. Keep a simple log: what you took, when, and how you felt afterward. Did you feel dizzy after taking your blood pressure pill? Did your confusion start after a new antidepressant? Bring this to your next appointment. Real-world data matters more than lab numbers sometimes.
The Future Is Personalized - But You Don’t Have to Wait
Researchers are now using AI to predict which drug combinations will cause problems for specific patients. One 2024 study showed machine learning models could predict adverse reactions with 89% accuracy - far better than traditional methods. The NIH just launched a public database of over 12 million patient records to help doctors find hidden risks.But you don’t need AI to protect yourself. Start now. Ask your doctor: “Could any of my conditions make this drug more dangerous?” “Is there a safer alternative?” “Could any of my other meds be causing these symptoms?”
The truth is, having multiple health conditions doesn’t mean you have to live with constant side effects. It just means you need to be smarter about how you take your medicine. With the right questions, the right team, and the right tools, you can take control - not just survive, but feel better.
Can having one chronic condition really double my risk of drug side effects?
Yes. Research shows patients with one or more chronic conditions are nearly three times more likely to experience an adverse drug reaction than those without. A 2017 study found 19.6% of patients with comorbidities had side effects, compared to just 7.6% of those without. This isn’t a small increase - it’s a major safety concern.
Why do I get dizzy when I take my blood pressure pill, but my friend doesn’t?
It’s likely because you have other conditions - like kidney disease, heart failure, or diabetes - that affect how your body processes the drug. These conditions slow down drug clearance, making the same dose too strong for you. Your friend might be healthier, so their body handles the same medication differently.
Is it safe to keep taking all my meds if I’m seeing multiple specialists?
Not without a full medication review. Patients with three or more conditions often see five or more doctors - and each one may prescribe without knowing what the others have ordered. This leads to dangerous overlaps. Ask for a pharmacist-led medication reconciliation to find duplicates, interactions, or unnecessary drugs.
What’s the most dangerous drug combination for someone with liver disease?
Acetaminophen (Tylenol) is the most common culprit. Even at normal doses, it can cause liver damage in people with cirrhosis or fatty liver disease. Other risky combinations include statins with certain antibiotics, and benzodiazepines with alcohol or opioids. Always check with your pharmacist before adding any new medication.
Can I reduce my meds instead of adding more?
Absolutely. Many older adults take medications they no longer need. The STOPP/START guidelines help doctors identify which drugs can be safely stopped. Deprescribing can reduce side effects, lower costs, and even improve quality of life. Ask your doctor: “Is there a drug I can stop?” - not just “What else can I take?”
Are there new tools to help doctors avoid dangerous drug combinations?
Yes. Electronic health systems now include comorbidity-aware alerts that flag risky prescriptions in real time. The NIH’s new Comorbidity-Drug Interaction Knowledgebase, launched in 2024, includes data from over 12 million patients and has already identified 217 new high-risk combinations. AI models are also predicting side effects with 89% accuracy - far better than older methods.
What to Do Next
If you or someone you care about has multiple health conditions, don’t wait for a crisis. Start today:- Make a complete list of every medication, supplement, and herb you take - including over-the-counter drugs and patches.
- Ask your primary care doctor to refer you to a clinical pharmacist for a medication review.
- Bring your list to every specialist appointment - and ask: “Is this still necessary given everything else I’m taking?”
- Keep a symptom journal for two weeks: note timing, dosage, and how you felt.
- Ask about deprescribing. You might feel better once you stop something you’ve been taking for years.
Medications are powerful - but they’re not magic. They work differently in every body. When you have comorbidities, you’re not just a patient. You’re a complex system. And you deserve care that matches that complexity.

pascal pantel
December 19, 2025 AT 09:30Let's cut through the fluff: polypharmacy in comorbid patients isn't just risky-it's systemic negligence. The liver's CYP450 system gets hammered by even modest drug loads, and when you throw in renal impairment, you're essentially running a pharmacokinetic simulation with broken variables. Studies show 47% of elderly polypharmacy cases involve at least one clinically significant interaction-many of which are preventable with basic CYP enzyme mapping. Yet we still rely on paper lists and handwritten notes. This isn't medicine-it's Russian roulette with pills.
Gloria Parraz
December 19, 2025 AT 10:32I’ve seen this firsthand with my mom-seven meds, three specialists, and zero coordination. She was dizzy all the time, thought it was just aging. Then a pharmacist sat down with us, mapped everything, and found three drugs that canceled each other out. One was a blood pressure pill that made her kidneys work overtime. She stopped it, and within a week, she was walking without the cane again. It’s not about more pills-it’s about less noise.
Sahil jassy
December 21, 2025 AT 07:06Kathryn Featherstone
December 22, 2025 AT 06:51It’s terrifying how often we treat comorbidities like separate problems instead of one interconnected system. I work in geriatrics, and I’ve seen patients prescribed anticoagulants, SSRIs, and NSAIDs-all without checking renal function. The side effects aren’t just side effects-they’re cascading failures. A little dizziness becomes a fall, then a fracture, then a hospital stay, then a nursing home. We’re not just prescribing drugs-we’re prescribing outcomes.
Nicole Rutherford
December 23, 2025 AT 14:15Let’s be real-this whole system is rigged. Big Pharma doesn’t test drugs on people with real comorbidities because then they’d have to admit most of their meds are dangerous for actual patients. They cherry-pick healthy 30-year-olds in trials, then sell the pills to 75-year-olds with kidney failure. And the FDA? They rubber-stamp it. You think the 89% AI accuracy number is magic? It’s just the tip of the iceberg. They’ve known this for decades. They just don’t care enough to fix it.
Chris Clark
December 24, 2025 AT 16:55Y’all talking about CYP enzymes like it’s rocket science. Honestly? It’s just biology. Liver’s tired? Kidneys slow? Your body ain’t built for 10 pills. I had a buddy on statins + ibuprofen + metformin-he got rhabdo. Doc said it was ‘rare.’ Nah. It’s common when you stack meds like Jenga blocks. Just ask your pharmacist. They see this every day. No PhD needed.
Dorine Anthony
December 26, 2025 AT 08:12I’m not a doctor, but I’ve been the one holding the medication log for my aunt for five years. She’s 82, has diabetes, heart disease, and depression. We started tracking symptoms in a notebook-when she felt foggy, when she got dizzy, what time she took each pill. Turned out her antidepressant was making her blood sugar crash. Changed the timing, lowered the dose, and suddenly she was laughing again. Sometimes the simplest tool is the most powerful.
William Storrs
December 27, 2025 AT 18:35Don’t give up. You’re not broken because you need meds. You’re just navigating a system that wasn’t built for people like you. But you’re not powerless. That pharmacist review? Do it. That symptom journal? Start today. That question-‘Can I stop anything?’-ask it like your life depends on it. Because it does. Small steps. One pill at a time. You’ve got this.
Janelle Moore
December 28, 2025 AT 05:18Wait… so you’re telling me the government and Big Pharma are secretly hiding that meds can kill people with multiple conditions? And they’re using AI to cover it up? That’s why your blood pressure pill makes you dizzy? They’re injecting tracking chips into the pills so they can monitor your body’s reaction and sell the data to insurance companies. They don’t want you to live longer-they want you to be a walking data point. I’ve seen the documents. They’re coming for your meds next.
Henry Marcus
December 28, 2025 AT 11:12EVERY SINGLE DRUG ON THE MARKET IS A TIME BOMB FOR PEOPLE WITH COMORBIDITIES-AND THEY KNOW IT. THE FDA’S ‘PROGRESS’? A SMOKE SCREEN. THEY’RE NOT TESTING ON REAL PATIENTS BECAUSE THE TRUTH WOULD BLOW UP THE ENTIRE PHARMA INDUSTRY! ACETAMINOPHEN? A LIVER KILLER. STATINS? MUSCLE MELTERS. ANTICOAGULANTS? BLEEDING TIME BOMBS. AND THEY’RE STILL PUSHING THEM ON GRANDMAS LIKE THEY’RE CANDY! I’VE BEEN TELLING PEOPLE FOR YEARS-THEY’RE NOT TREATING YOU. THEY’RE EXPERIMENTING.
Chris porto
December 30, 2025 AT 02:05It’s strange how we treat medicine like a checklist instead of a conversation. We add pills to fix symptoms without asking why the body is failing in the first place. Maybe the problem isn’t just the drugs-it’s the way we’ve stopped listening to the person behind the diagnosis. I’ve known patients who felt better not because of a new prescription, but because someone finally asked, ‘How are you really doing?’ Sometimes the most powerful drug is being seen.
William Liu
December 31, 2025 AT 10:16This is the kind of post that gives me hope. We’ve been told for so long that aging means more pills and more problems. But the truth? You can take back control. One question at a time. One review. One journal entry. You’re not helpless. You’re just waiting for someone to tell you it’s okay to ask for better. So ask. Keep asking. You deserve to feel good-not just survive.