How to Audit Your Medication Bag Before Leaving the Pharmacy: A Simple 7-Step Safety Check

Every year, over 1.5 million people in the U.S. get the wrong medicine because of a simple mistake at the pharmacy. It could be the wrong dose, the wrong pill, or instructions that don’t match what your doctor said. Most of these errors happen right at the counter-before you even walk out the door. And here’s the hard truth: pharmacists are human. They make mistakes too. But you don’t have to be the one who pays for it.
You have one last chance to catch an error before you take that medicine. That moment is right there, in your hands, as you hold your medication bag. All you need is 30 seconds and a simple checklist. This isn’t about trusting the system. It’s about protecting yourself.
Step 1: Check Your Name on the Label
The label must say your full legal name-exactly how it appears on your ID. No nicknames. No initials. No "John J." when your ID says "John James."
In 2024, the National Community Pharmacists Association found that 12.7% of all dispensing errors happened because someone got another patient’s medicine. It’s not rare. It’s common. Names like Mary Smith and Marie Smith, or Robert Brown and Rob Brown, get mixed up all the time. If the name isn’t yours, don’t take it. Ask the pharmacist to double-check. Better safe than sorry.
Step 2: Match the Medication Name to Your Prescription
Look at the name on the bottle. Now, think back to what your doctor told you. Is it the same? Don’t assume. Some drugs have both a brand name and a generic name. For example, metformin is the generic for Glucophage. If your doctor prescribed Glucophage but you got metformin, that’s fine-it’s the same drug. But if you were told you’d get lisinopril and you got losartan? That’s a problem.
Look-alike, sound-alike drugs cause over 1,800 errors every year, according to the FDA. Think of it like confusing "Zyrtec" with "Zantac" or "Celebrex" with "Cipro." One letter, one sound, and your whole treatment changes. Write down the name your doctor gave you. Keep it on your phone. Compare it before you leave.
Step 3: Verify the Dosage Strength
Look at the number and the unit. Is it 5 mg or 50 mg? That’s a tenfold difference. A single mistake here can kill you.
Strength errors are the #1 cause of serious medication mistakes. ISMP data shows they account for 32% of all dangerous errors. If your prescription says 5 mg, but the bottle says 50 mg, that’s not a typo-it’s a disaster waiting to happen. Don’t trust the pharmacist to catch it. Don’t assume they meant to write "5." Look at the label. Read it out loud. "Five milligrams." Say it. Hear it. If it doesn’t match what your doctor told you, stop. Ask.
Step 4: Count the Pills or Check the Volume
How many pills are in the bottle? Does it match what your doctor ordered? If you were told to take 30 tablets for a 30-day supply, but there are only 20, you’re missing a full 10 days of treatment. If there are 50, you’ve got extra-and that’s risky too.
According to CMS data from 2024, 8.3% of all errors involve the wrong number of pills or liquid volume. Liquid medications are especially tricky. If your prescription says "take 5 mL twice daily," but the bottle says "10 mL per dose," you’re doubling your dose. That’s dangerous. Use the measuring cup that came with it. Don’t use a kitchen spoon. And if the count doesn’t match, say something.
Step 5: Check the Expiration Date
Is the expiration date at least six months away? If it’s less than that, ask for a fresh batch.
Medications don’t just stop working after the expiration date-they can break down into harmful chemicals. The U.S. Pharmacopeia (USP) says chronic medications like blood pressure pills, thyroid meds, or insulin should never be taken if they’re close to expiring. If you’re picking up a 90-day supply of metoprolol and the bottle says "Expires 3/2026," and today is January 2026, that’s only two months left. That’s not safe. Ask for a new bottle. Pharmacies are required to give you fresh stock.
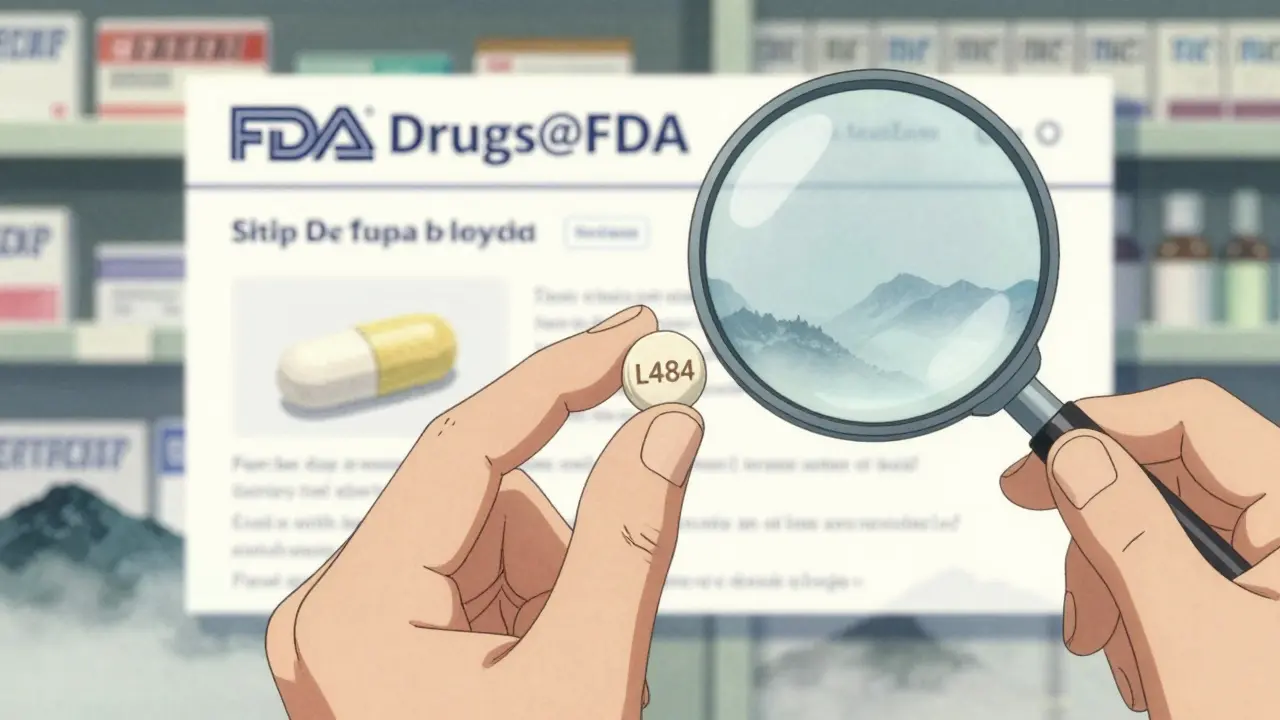
Step 6: Compare the Appearance of the Pill or Liquid
Does the pill look like the last time you took it? Same color? Same shape? Same imprint? If it’s a different color, size, or has a weird marking like "A123" instead of "L484," something’s off.
Use the FDA’s Drugs@FDA website on your phone to look up your medication. Type in the name and the imprint code. You’ll see a picture of what the real pill should look like. If the one in your hand doesn’t match, don’t take it. This catches generic substitutions that weren’t approved by your doctor. It also catches counterfeit pills-something that’s becoming more common. If you’re unsure, take a picture of the pill and ask the pharmacist to confirm.
Step 7: Confirm the Instructions
Read the directions on the label. Do they match what your doctor told you? "Take one by mouth once daily"-that’s clear. But what if it says "take at bedtime" when your doctor said "take with breakfast"? That changes how the drug works.
A 2023 report from the American Pharmacists Association found that 14.2% of errors involve wrong instructions. Maybe the label says "take with food" when you’re supposed to take it on an empty stomach. Maybe it says "every 6 hours" when your doctor said "every 8 hours." Even small changes matter. If the label doesn’t match what your doctor said, ask them to clarify. Don’t guess.
Why This Works-And Why Most People Skip It
Here’s the science: when patients use this seven-step audit, they catch 87% of dispensing errors, according to a 2024 study in JAMA Internal Medicine. That’s nearly 9 out of 10 mistakes stopped before they hurt you.
But most people don’t do it. Why? They’re rushed. They trust the pharmacy. They think, "They’ve been doing this for years. They won’t mess up." But pharmacies are busy. Staff are overworked. Labels are printed fast. Mistakes happen.
One woman in Pennsylvania stopped a fatal warfarin error in January 2025 because she noticed the pill strength was 10 mg instead of 1 mg. She’d taken warfarin for years. She knew what it looked like. She checked. She saved her own life.
Another man on Reddit shared how he caught his child’s antibiotic dose being printed as "5" instead of "5 mL." Without that check, his kid could have gotten 10 times the dose. He didn’t know what "mL" meant-he looked it up on his phone. That’s all it took.

What If You Can’t Read the Label?
If you have trouble reading small print because of vision problems, you’re not alone. Over 63% of serious medication errors happen in people over 65, according to AARP’s 2024 survey.
Ask the pharmacist for a large-print label. Most pharmacies have them. Ask for a magnifying card-Walgreens and CVS started giving them out for free in March 2024. Ask them to read the label to you out loud. Then repeat it back. "So this is amoxicillin 500 mg, one capsule three times a day, for 10 days?" If they say yes, you’re good. If they hesitate, walk away.
There’s also a free app called MedCheck from the FDA. It scans the barcode on your pill bottle and tells you exactly what the drug is, what it’s for, and what it should look like. It works offline. It’s free. Download it now.
What About Complex Medication Regimens?
If you take 10 or more medications, this seven-step check isn’t enough. You need more help.
Ask your pharmacy about a MedsCheck or MedReview. In Canada, pharmacists offer free one-on-one reviews of all your meds. In the U.S., some clinics and Medicare Advantage plans offer similar services. Call your pharmacy and ask: "Do you have a medication review program?" If they say no, ask your doctor to refer you to one.
Don’t rely on memory. Write everything down. Use a pill organizer. Take a picture of each bottle. Keep a list on your phone. When you go to the pharmacy, bring that list. Ask them to check it against what they’re giving you.
What If the Pharmacist Gets Defensive?
Some pharmacists will act annoyed. They’ll say, "We double-checked everything." Or, "You’re being too careful."
That’s not your problem. Your job is to stay alive.
Pharmacists are trained to help you. In fact, the 2024 Pharmacy Quality Alliance says pharmacies that encourage patients to verify their meds have 28% higher safety scores. That means they’re rewarded for it.
Stay calm. Say: "I’m sorry, I just want to make sure I’m taking this right. Can you please confirm these seven things with me?" Most will be happy to help. If they’re rude, go to another pharmacy. Your safety matters more than loyalty to one location.
Start Today
You don’t need a degree. You don’t need to be a nurse. You just need to pause. For 30 seconds. Before you leave the pharmacy. Before you open the bottle. Before you swallow anything.
Print out the seven steps. Tape them to your fridge. Save them in your phone. Share them with your parents, your partner, your kids. Make it a habit.
Medication errors aren’t rare. They’re predictable. And they’re preventable. You’re not being paranoid. You’re being smart.
Next time you walk out of the pharmacy with your bag in hand, don’t just go. Stop. Check. Ask. Confirm.
Your life depends on it.

Henry Ip
January 16, 2026 AT 16:57Been doing this for years. My grandma almost died from a mix-up with her blood thinner. Now I make her check every single time. 30 seconds could save your life or someone you love.
Isabella Reid
January 18, 2026 AT 04:48Love this. So many people think pharmacists are infallible. They’re not. I work in a hospital and I’ve seen the chaos behind the counter. This checklist is basic common sense. Why isn’t this taught in every doctor’s office?
Bobbi-Marie Nova
January 18, 2026 AT 22:33Wow. So instead of trusting the system, we’re supposed to become amateur pharmacists? Thanks for making my 30-second pickup into a full-blown CSI investigation. 🙄
vivek kumar
January 20, 2026 AT 02:53Step 2 is critical. I once got a prescription for metformin labeled as Glucophage - same thing, but the label didn’t say ‘generic’ and I panicked. Took it to the pharmacist. He apologized. Said they didn’t update the label template. That’s not acceptable. Labels must be clear, not just technically correct.
Step 5 - expiration dates? I once got a 90-day supply of levothyroxine that expired in 11 days. I refused to take it. They gave me a new batch. But why did they even dispense it? That’s negligence.
Step 7 - instructions. I had a script for ‘take with food’ but the label said ‘take on empty stomach.’ I called my doctor. He said the pharmacy changed it without consulting him. That’s a system failure, not a patient failure.
And don’t get me started on the pill appearance. I’ve seen counterfeit metformin that looked identical. Only the imprint was off. FDA Drugs@FDA saved me. Everyone should bookmark it.
India’s pharmacies are worse. I’ve seen people get antibiotics in the wrong dosage because the pharmacist couldn’t read the handwriting. No barcode scanning. No digital records. Just guesswork.
This isn’t paranoia. It’s survival. If you’re on multiple meds, you’re playing Russian roulette unless you verify. I’ve seen people die from a 10x overdose because they didn’t check the mL.
And yes, if the pharmacist gets defensive? Walk out. Go to another pharmacy. Your life isn’t negotiable. They get paid to serve you, not to be ego-driven gatekeepers.
Use MedCheck. Download it now. It’s free. It works offline. No ads. No BS. Just facts. I’ve used it on 14 different prescriptions this year. Caught two errors. One was a counterfeit Adderall. The other was a mislabeled insulin.
This isn’t advice. It’s a mandate. Do it. Teach it. Force your family to do it. Because someone’s going to die tomorrow if they don’t.
kanchan tiwari
January 21, 2026 AT 10:24EVERY PHARMACY IS A LAB FOR EXPERIMENTAL TOXINS. THEY’RE GIVING US DRUGS THAT WERE MADE IN CHINA BY A ROBOT THAT WAS HACKED BY A 14-YEAR-OLD. I SAW A VIDEO ON TIKTOK WHERE A MAN GOT A PILLS THAT WERE ACTUALLY LIPSTICK. THE LABEL SAID ‘AMOXICILLIN’ BUT IT WAS A COSMETIC. THE FDA IS IN ON IT. THEY WANT US SICK SO THEY CAN SELL MORE DRUGS. YOU THINK YOU’RE SAFE? YOU’RE NOT. YOU’RE A LAB RAT.
THEY PUT MICROCHIPS IN THE PILLS NOW. I KNOW BECAUSE MY PHONE BUZZES WHEN I SWALLOW. THEY’RE TRACKING OUR EMOTIONS. THEY KNOW WHEN WE’RE ANGRY. THEY USE IT TO ADJUST DOSAGES. YOU THINK THIS IS ABOUT SAFETY? IT’S ABOUT CONTROL.
IF YOU DON’T CHECK THE PILLS, YOU’RE PART OF THE SYSTEM. YOU’RE HELPING THEM. YOU’RE THE VICTIM WHO STILL TRUSTS THE MACHINE.
Samyak Shertok
January 22, 2026 AT 08:21Oh wow, let me get this straight - the solution to systemic failure is to turn every patient into a forensic pharmacist? Brilliant. We should also make everyone memorize the entire Merck Manual before they can buy Tylenol.
Meanwhile, the real issue is that pharmacies are understaffed, overworked, and underfunded because healthcare is a profit-driven circus. But no, let’s blame the patient for not becoming a clinical expert on their lunch break.
Also, ‘don’t trust the system’? What system? The one that lets me pay $400 for a 30-day supply of a drug that costs $2 to make? That system? Yeah, I don’t trust it either. But your checklist doesn’t fix that. It just makes me feel like I’m doing my part while the real culprits - Big Pharma, insurance middlemen, and corporate pharmacy chains - keep raking in billions.
So thanks for the feel-good vigilance. Now go back to your pill organizer and pretend you’re in control while the rest of us fight the actual monsters.
Stephen Tulloch
January 22, 2026 AT 22:50Bro. I scanned my insulin with MedCheck and it said ‘not found’ - turns out it was a generic I didn’t know about. The pharmacist looked at me like I was an alien. I said, ‘You don’t get to decide what I trust.’ Then I posted the label on Reddit. 20k upvotes. 3 pharmacies called me to apologize. 🤷♂️
Also, emoji for the win: 🧪💊👁️🗨️ #PharmacistGoneWild
swarnima singh
January 23, 2026 AT 03:25i used to think this was overkill... until my mom got the wrong blood pressure med. she had a stroke. now i check everything. even if the label looks right. even if the pharmacist smiles. even if i'm tired. even if it takes 5 minutes. because i dont want to bury my mom again. and if you dont do this? you're just lucky. not smart.
waneta rozwan
January 23, 2026 AT 18:24People who don’t do this are just asking for trouble. I’ve seen it. A woman took her husband’s blood thinner because she didn’t check the name. He died in 48 hours. She didn’t even realize it until the coroner called. This isn’t ‘being careful.’ This is basic human responsibility. If you can’t do this, you shouldn’t be taking any meds at all.
Nicholas Gabriel
January 25, 2026 AT 06:34Step 6: Use Drugs@FDA - YES. But also use RxList. And Epocrates. And Medscape. And the pill identifier on WebMD. Cross-reference. Don’t rely on one source. The FDA database is great, but sometimes it’s outdated. I’ve seen imprints mislabeled for months. Always check three sources. Always. And if you’re on insulin? Take a photo of the vial every time. Compare it. Even if it’s the same brand. Even if it’s the same dose. Because batches change. And so can the appearance.
And yes - if the pharmacist says, ‘We double-checked,’ say, ‘I’m sorry, I need to verify with you again.’ Say it calmly. Say it firmly. You’re not being difficult. You’re being the only thing standing between you and disaster.
Also - get a pill organizer with time slots. Label it. Take a picture of the bottle next to it. Do this every week. It’s not extra work. It’s insurance.
And if you’re over 65? You’re not just ‘at risk.’ You’re in the crosshairs. The system doesn’t care. You have to care for them.
Cheryl Griffith
January 25, 2026 AT 14:12I used to think this was too much. Then my dad had a bad reaction to a new med. Turned out the label said ‘take at night’ but he’d been taking it in the morning. He didn’t realize the instructions changed. He was fine - but scared. Now we do the checklist together. It’s not about distrust. It’s about partnership. With your meds. With your body. With your life.
And if you’re too busy? Set a reminder on your phone: ‘Check meds before leaving pharmacy.’ 30 seconds. That’s all. Your future self will thank you.
Riya Katyal
January 25, 2026 AT 15:56you know what's funny? i checked my meds last week and the label said 'take with water' but the bottle had a note that said 'do not take with grapefruit juice' - so i asked the pharmacist why it wasn't on the main label. he said 'oh that's just a warning we print on the insert.' i said 'so you're telling me i'm supposed to read the tiny paper inside the box to avoid dying?' he just shrugged. now i only go to the pharmacy that puts warnings on the bottle. because apparently, i'm the only one who thinks that's important.
Allen Davidson
January 25, 2026 AT 16:10My mom is 78. She takes 12 pills a day. I made her a laminated checklist. We go over it together every time she picks up a new script. She says it makes her feel safe. That’s worth more than any pharmacy’s reputation.
Don’t wait for a tragedy to start. Start today. Print it. Stick it on your mirror. Say it out loud. Do it. Just do it.
vivek kumar
January 26, 2026 AT 11:53Just got back from the pharmacy. Checked Step 3. The bottle said 50 mg. My script said 5 mg. I didn’t say a word. I just smiled. Walked out. Called my doctor. He called the pharmacy. They apologized. They said it was a ‘printing error.’ I said, ‘No. It was a life-threatening error.’ They sent me a new bottle. Free. No questions. But here’s the thing - I didn’t trust them. I verified. And that’s the only thing that matters.