How to Avoid Overdose When Restarting a Medication After a Break

When you stop taking a medication-whether it’s for opioids, benzodiazepines, antidepressants, or painkillers-and then start again later, your body doesn’t remember how to handle the same dose. That’s the quiet, deadly truth behind many overdoses after a break. People think, “I used to take this just fine,” so they go back to their old dose. But their body has changed. Their tolerance is gone. And that’s when things go wrong.
Why Your Body Can’t Handle the Same Dose Anymore
Tolerance isn’t just a buzzword. It’s a real, measurable change in your body’s response to a drug. When you take a medication regularly, your brain and liver adapt. You need more to feel the same effect. But when you stop-even for a few days-those adaptations start to reverse. For opioids like oxycodone or heroin, tolerance can drop by 50% in under a week. For methadone, it can vanish in just 3 to 5 days. That means a dose that once felt manageable now floods your system like a tidal wave. This isn’t just theory. In 2014, actor Philip Seymour Hoffman died of an overdose after 23 years of sobriety. He wasn’t using heavily. He wasn’t chasing a high. He took the same dose he used to take years before-and his body couldn’t process it. His lungs stopped. He wasn’t a reckless user. He was someone who didn’t know his body had changed. The same thing happens with benzodiazepines like Xanax or sleep aids like zolpidem. Your nervous system calms down when you’re off the drug. When you restart at your old dose, your breathing slows too much. Your heart rate drops. You pass out. And if you’re alone, no one finds you in time.Which Medications Are Most Dangerous to Restart?
Some medications carry far higher risks than others when restarted after a break:- Opioids (oxycodone, hydrocodone, fentanyl, methadone): Highest risk. Even small doses can cause fatal respiratory depression after just a few days off.
- Benzodiazepines (alprazolam, diazepam, clonazepam): Rapid tolerance loss. Restarting at old doses can cause seizures, coma, or stopped breathing.
- Antidepressants (SSRIs, SNRIs like sertraline, venlafaxine): Risk of serotonin syndrome if restarted too soon after MAOIs or other serotonergic drugs.
- MAOIs (phenelzine, tranylcypromine): Must wait at least 14 days before switching to SSRIs or SNRIs. Restarting too soon can trigger life-threatening serotonin toxicity.
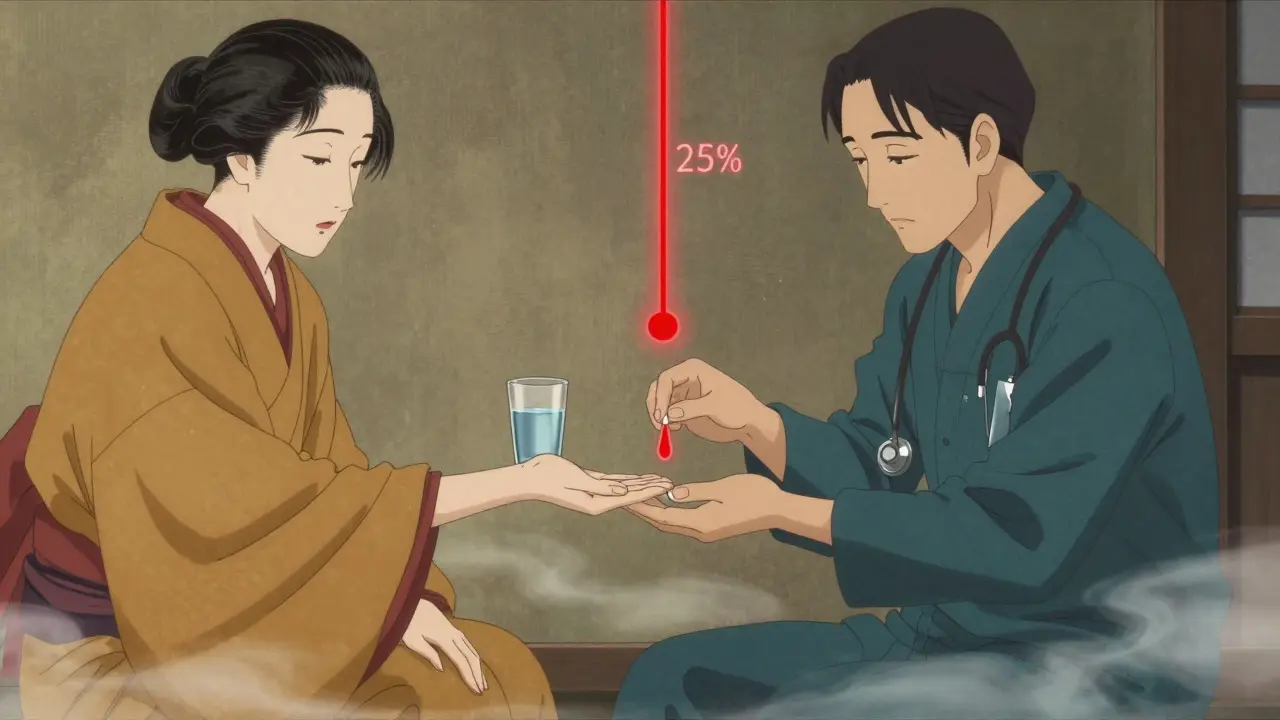
The Safe Restart Protocol: Start Low, Go Slow
There’s one rule that saves lives: start at 25% to 50% of your previous dose. Then wait. For opioids:- If you were taking 40mg of oxycodone daily, start with 10mg.
- Wait 24 to 48 hours before increasing.
- Only increase by 25% at a time.
- Monitor for drowsiness, slow breathing (fewer than 12 breaths per minute), or pinpoint pupils.
- If you used to take 2mg of lorazepam, start with 0.5mg.
- Wait 3 days before considering another increase.
- Never restart at full dose-even if you feel fine.
- If you were on venlafaxine 150mg and stopped for more than a week, start with 37.5mg.
- Wait 7 days before increasing.
- If you were on an MAOI, wait at least 14 days before starting any SSRI or SNRI.
Never Restart Alone
The most dangerous time to restart medication is when you’re alone. That’s when no one notices if you stop breathing. That’s when no one calls 911. That’s when naloxone could save your life-but only if it’s nearby and someone knows how to use it. Always have naloxone on hand if you’re restarting opioids. It’s not just for emergencies-it’s a safety net. Keep it in your wallet, your car, your bedside drawer. Teach a friend, a family member, or your roommate how to use it. The Washington State guidelines say this clearly: “Naloxone should be shared with a trusted person before restarting opioid therapy.” If you’re restarting any CNS depressant-opioids, benzos, sleep meds-have someone check on you every few hours for the first 24 to 48 hours. Ask them to watch for:- Slurred speech
- Extreme drowsiness
- Slow or shallow breathing
- Unresponsiveness
When Medical Supervision Isn’t Optional
Some situations demand professional help. If you’ve been off medication for:- More than 7 days and you’re restarting opioids
- More than 14 days and you’re restarting an MAOI or switching antidepressants
- After being released from jail, prison, or a treatment facility

What to Do If You’ve Already Restarted and Feel Off
You took your old dose. You feel dizzy. Your breathing feels slow. You’re not sure if it’s normal. Stop. Don’t take more. Don’t wait it out. Call emergency services immediately. If you have naloxone, use it-even if you’re not sure it’s an overdose. Naloxone won’t hurt you if you don’t need it. But if you’re overdosing, it can bring you back. Afterward, talk to your doctor. Don’t hide it. Don’t feel guilty. This happens to people all the time. The goal isn’t to punish you-it’s to make sure you don’t do it again.What’s New in Overdose Prevention
In early 2024, the American Society of Addiction Medicine released new guidelines that include a 10-point scoring system to determine safe restart doses based on:- How long you were off the medication
- Your previous daily dose
- Your age and liver health
- Whether you use alcohol or other sedatives
The Bottom Line
Restarting medication after a break isn’t about willpower. It’s about biology. Your body forgets how to handle the drug. Your tolerance resets. The dose that once kept you stable can kill you now. Don’t guess. Don’t assume. Don’t rush. Start low. Go slow. Have naloxone. Tell someone. Get professional help if you can. This isn’t fear-mongering. It’s science. And it’s the difference between life and death.How long does it take to lose tolerance after stopping medication?
Tolerance loss happens fast. For short-acting opioids like heroin or oxycodone, it can begin within 24 hours and drop significantly in 3 to 5 days. For methadone, tolerance can vanish in 3 to 7 days. Benzodiazepines lose tolerance within 5 to 10 days. Even antidepressants can see changes in metabolism within a week. The longer you’re off, the more your body forgets how to handle the drug.
Can I restart my old dose if I feel fine after a few days?
No. Feeling fine doesn’t mean your body is ready. Tolerance is invisible. You might feel alert, but your breathing could already be slowing. Your liver may not be metabolizing the drug properly. That’s why medical guidelines say to start at 25% to 50% of your old dose-even if you think you can handle more. What felt normal before can now be deadly.
Is naloxone only for people who use street drugs?
No. Naloxone is for anyone restarting prescription opioids, even if they were prescribed legally. Many overdoses happen to people on painkillers after surgery, hospital stays, or breaks in treatment. Naloxone is not for “addicts”-it’s for anyone at risk of respiratory depression. It’s a medical safety tool, like a fire extinguisher.
What if I’m restarting an antidepressant after stopping for a month?
Start at 25% of your previous dose and wait at least 7 days before increasing. If you were on an MAOI before, wait 14 days before starting any SSRI or SNRI to avoid serotonin syndrome. Symptoms include agitation, rapid heart rate, high fever, and muscle rigidity. These can be fatal. Don’t rush-your brain needs time to readjust.
Can I restart medication after being in jail or prison?
Yes-but only under medical supervision. Over 60% of fatal overdoses after incarceration happen in the first 72 hours. Prisons often stop medications, and tolerance drops quickly. Don’t rely on your old dose. Ask for a harm reduction plan before release. Many states now have programs that connect people to naloxone and supervised restart protocols before they walk out the door.
What if I don’t have access to a doctor?
Start at 25% of your previous dose and wait at least 48 hours before increasing. Never restart alone. Have someone nearby who knows how to use naloxone. Call a local pharmacy-they can often advise on safe dosing and may provide naloxone without a prescription. In New Zealand, Australia, Canada, and parts of the U.S., naloxone is available over the counter. Use it. It’s not risky. It’s lifesaving.

Alexandra Enns
January 24, 2026 AT 12:34Okay but let’s be real-this whole post is just fear porn dressed up as medical advice. I’ve been off oxycodone for 10 months and hit my old dose of 60mg and felt fine. My liver’s a tank. My tolerance didn’t ‘vanish.’ You’re treating people like fragile glass figurines. Some of us don’t need a 25% reduction-we need a damn reality check.
Marie-Pier D.
January 25, 2026 AT 03:10My brother died from this exact thing after his surgery. He was on 30mg oxycodone daily, took a 12-day break for the hospital, then took his old dose at home… and never woke up. 💔 I’m so glad someone’s talking about this. Please, if you’re restarting-start at 1/4. I beg you. Naloxone isn’t optional. It’s your lifeline. ❤️
Sawyer Vitela
January 25, 2026 AT 20:3170% lower risk? Source? Washington State guidelines? Name the study. This isn’t evidence-it’s anecdotal propaganda. Tolerance decay curves vary by individual metabolism, CYP450 polymorphisms, and half-life of the compound. You’re oversimplifying pharmacokinetics for clicks.
Izzy Hadala
January 27, 2026 AT 18:11While the general sentiment of this post is commendable, one must acknowledge the absence of peer-reviewed longitudinal data correlating dose reduction protocols with mortality outcomes. The referenced 70% reduction statistic, though compelling, lacks citation to a validated cohort study. Furthermore, the assertion that tolerance 'vanishes' in 3–5 days for methadone contradicts the pharmacodynamic half-life of its active metabolites, which persist for up to 14 days in some individuals. A more nuanced discussion is warranted.
Elizabeth Cannon
January 28, 2026 AT 03:34omg this is so important!! i had a friend almost die last year bc she thought she could just jump back on her 100mg venlafaxine after 3 weeks off. she ended up in the ER with serotonin syndrome. please, if you’re reading this-DON’T BE THAT PERSON. start low, tell someone, get naloxone if you’re on opioids. it’s not weak, it’s smart. 💪
blackbelt security
January 29, 2026 AT 04:37Been there. Done that. Lost friends. Now I carry naloxone in my wallet and my car. If you’re restarting, you’re not weak-you’re responsible. Don’t wait for a tragedy to learn this lesson.
Patrick Gornik
January 30, 2026 AT 22:59Let’s deconstruct the metaphysics of tolerance: the body doesn’t ‘forget’-it re-optimizes. The ghost of your old neurochemistry haunts your synapses, whispering, ‘Remember this?’ But the synaptic pruning has already begun. You are not the same person who last held that pill. You are a new organism in an old skin. The dose is not a relic-it’s a tombstone. And if you resurrect it without ritual, without humility, without the sacred pause-you are not a patient. You are a sacrilege against biology itself.
Karen Conlin
February 1, 2026 AT 05:35I work in harm reduction in rural Ohio, and I’ve seen this play out too many times. People come in after a stint in jail or after a hospital stay, thinking they can just pick up where they left off. They don’t realize their tolerance’s gone. We hand out naloxone kits, teach families how to use them, and we always, always say: start at 25%. That’s not advice-it’s a lifeline. And if you’re restarting an antidepressant? Wait. Wait seven days. Your brain’s rewiring. Don’t rush it. You’re not failing-you’re healing. And you deserve to do it safely.
Sushrita Chakraborty
February 1, 2026 AT 12:04This is an exceptionally well-researched and compassionate piece. The inclusion of jurisdiction-specific resources-particularly for New Zealand, Australia, Canada, and the United States-is both pragmatic and globally considerate. The emphasis on supervised restarts following incarceration is not merely clinical; it is profoundly ethical. I would urge all healthcare providers, particularly in low-resource settings, to adopt these protocols as standard practice. The data presented is not speculative-it is, in fact, life-saving. Thank you for this vital contribution to public health discourse.