How to Prevent and Manage Antibiotic-Induced Diarrhea and C. diff Infection
C. diff Risk Assessment Tool
C. diff Risk Assessment
This tool helps you understand your risk of developing C. diff infection after antibiotic treatment based on CDC guidelines and recent research.
Your Risk Assessment
When you take an antibiotic, you expect it to kill the bad bacteria making you sick. But what you might not realize is that it’s also wiping out the good bacteria in your gut - the ones that keep your digestion running smoothly. For some people, this disruption leads to diarrhea. For others, it opens the door to something far more dangerous: Clostridioides difficile infection, or C. diff.
C. diff isn’t just a bad case of stomach upset. It’s a serious infection that can cause severe diarrhea, fever, abdominal pain, and in worst cases, life-threatening colon damage. About 1 in 5 people who get antibiotic-associated diarrhea end up with C. diff, according to CDC data. And it’s not just hospital patients - community cases are rising. In 2023, the CDC labeled C. diff an urgent threat, meaning it’s not going away anytime soon.
What Causes C. diff After Antibiotics?
Your gut is home to trillions of bacteria - a complex ecosystem that helps digest food, makes vitamins, and keeps harmful microbes in check. When you take antibiotics, especially broad-spectrum ones like fluoroquinolones, clindamycin, or cephalosporins, you don’t just target the infection. You also wipe out protective bacteria like Bacteroides and Faecalibacterium. That’s when C. diff, which may have been lying dormant in your gut or picked up from a contaminated surface, gets its chance to take over.
C. diff doesn’t cause harm by itself. It’s the toxins it produces - toxin A and toxin B - that attack the lining of your colon. This leads to inflammation, fluid leakage, and the classic symptom: watery diarrhea, sometimes 10 to 15 times a day. The spores of C. diff are tough. They can survive on doorknobs, bed rails, and toilets for months. That’s why handwashing with soap and water - not just hand sanitizer - is critical. Alcohol-based gels don’t kill the spores.
Who’s at Highest Risk?
Not everyone who takes antibiotics gets C. diff. But some people are far more vulnerable:
- People over 65 - age weakens the immune system and gut defenses
- Those who’ve been in a hospital or nursing home for more than 72 hours
- People on multiple antibiotics at once or for longer than 10 days
- Those with weakened immune systems from cancer treatment, organ transplants, or chronic illness
- Patients who’ve had recent bowel surgery or a feeding tube
Even healthy adults can get it. A 2023 study found that nearly 25% of community-acquired C. diff cases happened in people with no recent hospital stay. That means you don’t have to be sick in a hospital to catch it - you just need to have taken an antibiotic.
How Is It Diagnosed?
Doctors can’t tell C. diff from regular diarrhea just by symptoms. That’s why testing is essential - but it’s not simple. A stool test is required, and it must be unformed (not solid). If you’ve taken a laxative in the last 48 hours, the test won’t work.
Most labs use a two-step process: first, they screen for a protein called GDH that C. diff produces. If that’s positive, they test for the actual toxins. Sometimes they use a DNA test (NAAT) to detect the bacteria’s genes. But here’s the catch: you can test positive for C. diff and not have an active infection. Some people carry the bacteria without symptoms. That’s why doctors look at your whole picture - symptoms, recent antibiotics, and test results - before making a diagnosis.
Too many patients are misdiagnosed. One analysis of over 1,000 online patient posts found that nearly 4 in 10 were first told they had a virus or IBS. Delayed diagnosis means longer illness and higher risk of complications.
How Is C. diff Treated?
Treatment depends on how severe your infection is and whether it’s your first episode or a recurrence.
First-time, non-severe C. diff: Oral vancomycin (125 mg four times a day for 10 days) or fidaxomicin (200 mg twice daily for 10 days) are now the standard. Metronidazole is no longer recommended as first-line - studies show it fails in 30-40% of cases now, compared to just 5-15% a decade ago.
Severe C. diff: Defined by a white blood cell count over 15,000 or rising creatinine levels. Vancomycin or fidaxomicin are still first-choice, but higher doses may be needed. In critical cases with ileus or toxic megacolon, doctors may add IV metronidazole and even give vancomycin as a rectal enema.
Recurrent C. diff: This is where things get tricky. About 1 in 5 people get it again after treatment. For the first recurrence, the same antibiotic may be tried again. But for second or third recurrences, a tapered vancomycin schedule is often used: daily for 10-14 days, then every other day for a week, then once every 2-3 days for up to 8 weeks. This slow reduction helps the good bacteria come back without triggering another flare.
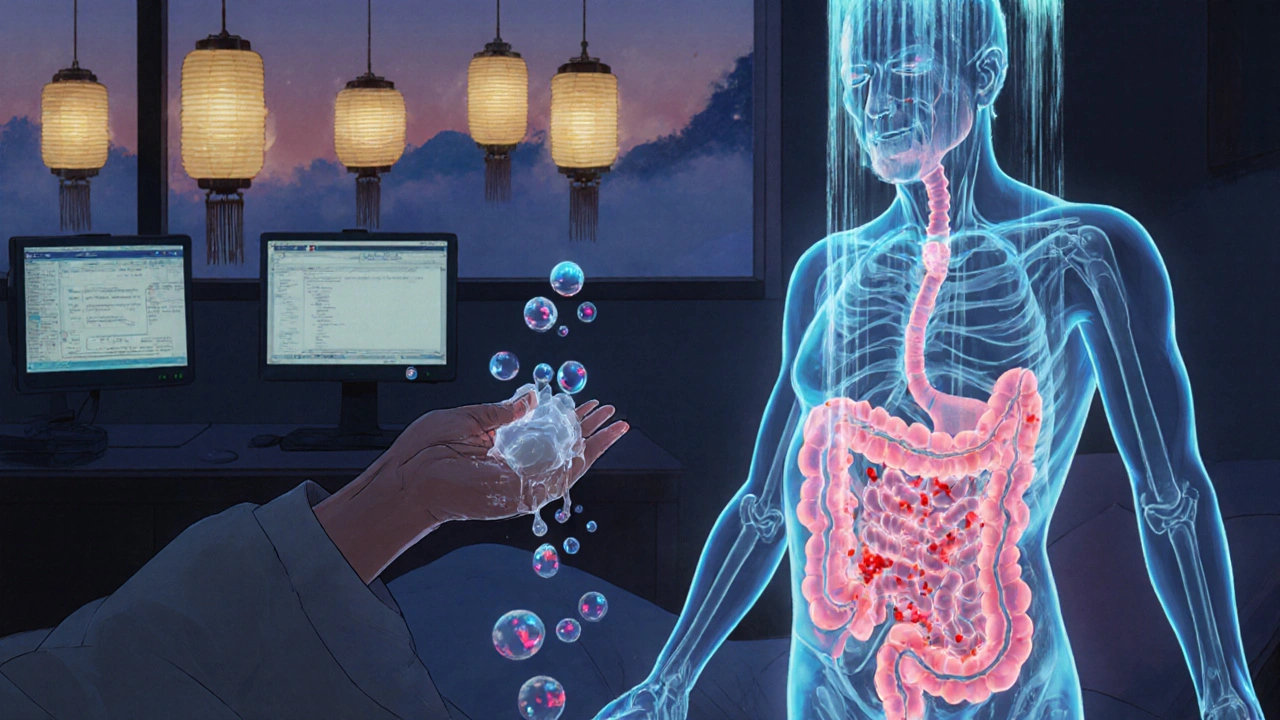
Fecal microbiota transplantation (FMT) - a procedure where healthy donor stool is placed into the patient’s colon - is now FDA-approved for recurrent C. diff after antibiotic failure. Studies show it works in 85-90% of cases. A newer option, Vowst (a capsule of bacterial spores), was approved in April 2023 and offers a non-invasive alternative. One patient on a support forum wrote, “After seven recurrences over 18 months, one FMT cleared me for good. I wish I hadn’t waited so long.”
Another tool is bezlotoxumab (Zinplava), a monoclonal antibody that neutralizes one of C. diff’s toxins. Given as a single IV infusion alongside antibiotics, it cuts recurrence risk by 10 percentage points. But it’s expensive - over $20,000 per dose - and only used for high-risk patients.
What NOT to Do
Many people reach for anti-diarrheal meds like loperamide (Imodium) to stop the runs. That’s a mistake. These drugs slow down your gut, trapping the toxins inside your colon. That can make the infection worse and increase the risk of toxic megacolon - a life-threatening condition where the colon swells and can rupture.
Don’t keep taking the antibiotic that caused the problem unless your doctor says to. Stopping the trigger is often the most important step. And don’t ignore symptoms just because you think it’s “just a stomach bug.” If diarrhea starts during or right after antibiotics, get tested.

How to Prevent C. diff Before It Starts
The best way to avoid C. diff is to avoid unnecessary antibiotics. The CDC estimates that 30-50% of antibiotic prescriptions in hospitals are inappropriate - given for viral infections like colds or flu, where they do nothing.
Ask your doctor: “Is this antibiotic really needed?” and “Is there a narrower-spectrum option?” If you’re prescribed one, take it exactly as directed - no skipping doses, no stopping early unless your doctor says so. But also, don’t demand antibiotics for a sore throat if your doctor says it’s viral.
At home, clean surfaces with EPA-registered sporicidal cleaners (look for List K on the label). Regular disinfectants won’t kill C. diff spores. Wash your hands with soap and water after using the bathroom, before eating, and after touching anything in a hospital.
Probiotics? The evidence is mixed. Some studies suggest Saccharomyces boulardii or Lactobacillus rhamnosus GG might reduce risk by up to 60% in high-risk patients. But the IDSA guidelines don’t recommend them routinely because results aren’t consistent. If you want to try one, talk to your doctor first.
Recovery and What Comes After
Most people feel better within a few days of starting the right antibiotic. But recovery isn’t just about stopping diarrhea. Many report lingering fatigue, brain fog, and food intolerances for weeks or even months. One patient survey found 37% still felt tired after the diarrhea ended. 82% had to avoid dairy, spicy foods, or caffeine during recovery.
Rebuilding your gut microbiome takes time. Eating fiber-rich foods - oats, bananas, apples, legumes - helps feed the good bacteria. Fermented foods like yogurt with live cultures, kefir, sauerkraut, and kimchi may help, though they’re not a cure. Avoid sugar and processed foods - they feed the bad bugs.
If you’ve had multiple recurrences, your doctor may recommend a microbiome-focused approach: FMT, Vowst, or future therapies like ridinilazole, which showed better results than vancomycin in recent trials. The goal isn’t just to kill C. diff - it’s to restore your gut’s natural balance so it can defend itself.
The Bigger Picture
C. diff doesn’t just hurt individuals - it strains the whole healthcare system. In the U.S., it costs nearly $5 billion a year. Hospitals with strong antibiotic stewardship programs - meaning they track and limit unnecessary antibiotic use - have cut C. diff rates by 26% in just six years.
But progress is uneven. Only 45% of U.S. hospitals stock fidaxomicin because it’s so expensive. That means patients in smaller or underfunded facilities often get older, less effective drugs. Access to FMT and newer treatments is even more limited.
The future is promising: rapid diagnostic tests, microbiome-sparing antibiotics, and personalized treatments based on your gut bacteria profile are on the horizon. But until then, the best tools we have are simple: use antibiotics wisely, wash your hands, and know the signs.
If you’ve had C. diff before, tell every doctor you see - even your dentist. It changes how they approach any future treatment. And if you’re on antibiotics now and start having diarrhea, don’t wait. Call your provider. Early action saves lives.
Can probiotics prevent C. diff infection?
Some studies suggest certain probiotics - like Saccharomyces boulardii and Lactobacillus rhamnosus GG - may reduce the risk of C. diff by about 60% in people taking antibiotics, especially in hospital settings. But the evidence isn’t strong or consistent enough for major medical groups like the Infectious Diseases Society of America to recommend them for everyone. If you’re considering probiotics, talk to your doctor first - they’re not a substitute for proper antibiotic use or hygiene.
Is C. diff contagious?
Yes. C. diff spreads through spores in feces. If someone with the infection doesn’t wash their hands after using the bathroom, they can leave spores on surfaces like doorknobs, toilets, or bed rails. Others touch those surfaces and then touch their mouth - and get infected. That’s why soap and water handwashing is critical. Alcohol-based sanitizers don’t kill the spores.
Can you get C. diff without taking antibiotics?
Yes. While antibiotics are the biggest risk factor, about 25% of community cases happen in people who haven’t taken antibiotics recently. Other factors like advanced age, recent hospital stays, weakened immune systems, or chronic illness can still allow C. diff to take hold. Spores can be picked up from contaminated environments - even from food or water in rare cases.
Why is metronidazole no longer the first treatment for C. diff?
Metronidazole was once the go-to drug, but over time, studies showed it was failing more often - up to 30-40% of cases now. Vancomycin and fidaxomicin are more effective at clearing the infection and have lower recurrence rates. The CDC and IDSA updated their guidelines in 2017 to reflect this, removing metronidazole from first-line use. It’s now only used if the other drugs aren’t available.
How long does it take to recover from C. diff?
Most people start feeling better within 2-3 days of starting the right antibiotic. Diarrhea usually stops within a week. But full recovery - including energy levels and gut health - can take weeks or months. Fatigue and brain fog are common aftereffects. Some people develop food sensitivities and need to avoid dairy or spicy foods for a while. Recurrence is possible, especially if you’re on more antibiotics soon after.
What’s the difference between vancomycin and fidaxomicin?
Both are effective for treating C. diff, but fidaxomicin is more targeted - it stays in the gut and doesn’t disrupt other good bacteria as much. This leads to fewer recurrences: about 13% with fidaxomicin versus 22% with vancomycin. However, fidaxomicin costs over $3,000 per course, while vancomycin is around $1,650. Many hospitals don’t stock fidaxomicin because of the price, so vancomycin remains the more common choice.
Is fecal microbiota transplant (FMT) safe?
Yes, when done through approved methods. FDA-approved FMT products like Rebyota and Vowst use carefully screened donor stool tested for over 50 pathogens. The procedure has a 90% success rate for recurrent C. diff. Side effects are usually mild - bloating, cramping, or temporary diarrhea. Serious risks are rare. It’s not a first-line treatment, but for people with multiple recurrences, it’s often life-changing.

Lexi Brinkley
November 7, 2025 AT 15:35Jim Oliver
November 8, 2025 AT 03:44Brierly Davis
November 9, 2025 AT 06:13Amber O'Sullivan
November 10, 2025 AT 11:39William Priest
November 11, 2025 AT 08:17Edward Weaver
November 12, 2025 AT 17:51Ryan Masuga
November 14, 2025 AT 13:12Jennifer Bedrosian
November 15, 2025 AT 05:28Lashonda Rene
November 17, 2025 AT 05:25Beth Banham
November 18, 2025 AT 02:03Andy Slack
November 19, 2025 AT 09:40