How to Prevent Heat-Related Medication Problems in Seniors
Why Heat Turns Ordinary Medications into Hidden Dangers for Seniors
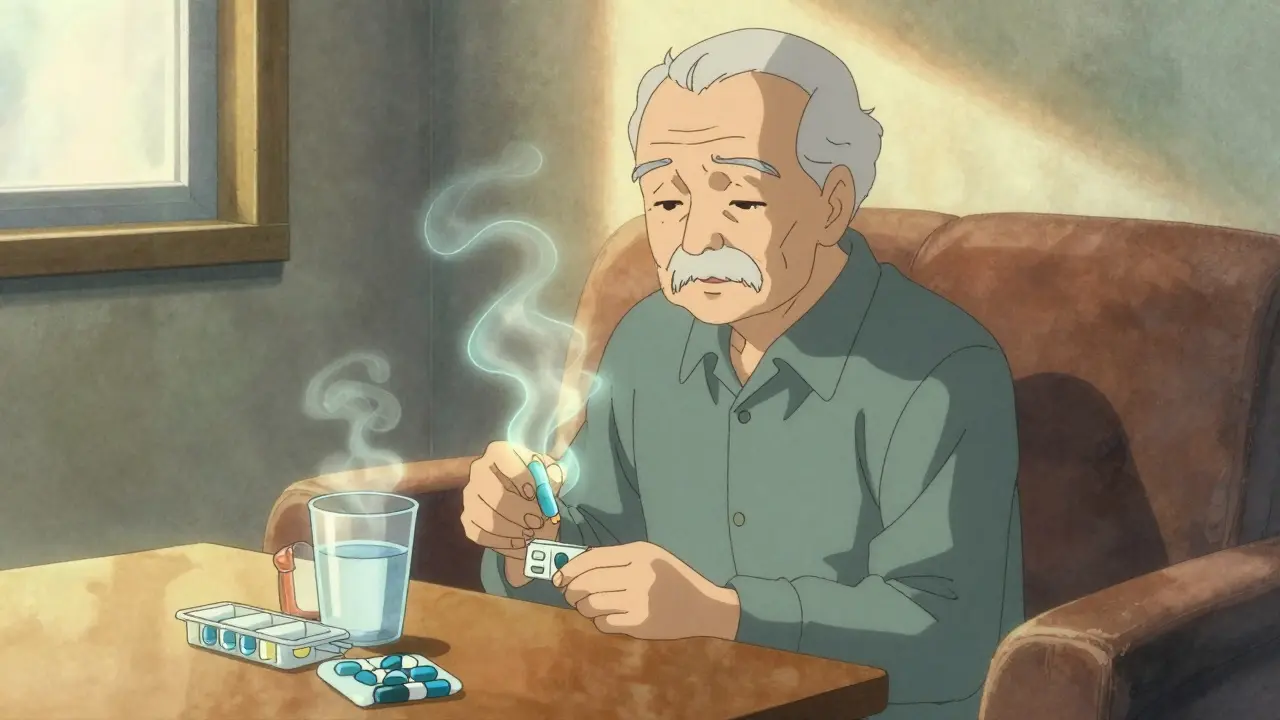
When the temperature rises, most people think about drinking more water or turning on the fan. But for seniors taking certain medications, heat isn’t just uncomfortable-it’s life-threatening. A 78-year-old on diuretics might not feel thirsty, even as their body loses fluids faster than they can replace them. Someone on an antipsychotic might not sweat at all, letting their core temperature climb silently to dangerous levels. These aren’t rare cases. According to the CDC, heat-related medication problems are behind a growing number of emergency visits and deaths among older adults, especially during summer heat waves.
The problem isn’t just the heat. It’s what happens when heat meets common prescriptions. About 87% of seniors over 65 take two or more medications daily. Many of these drugs-like those for high blood pressure, heart failure, or depression-interfere with how the body cools itself. They reduce thirst, block sweating, throw off electrolytes, or make skin more sensitive to the sun. When these effects combine with rising temperatures, the body can’t keep up. And because aging naturally slows down temperature regulation, seniors are caught in a perfect storm.
Medications That Turn Up the Heat Risk
Not all medications are equally risky, but some are silent danger zones during hot weather. Here are the top offenders:
- Diuretics (like Hydrochlorothiazide, Furosemide): These are called "water pills" because they help the body get rid of extra fluid. But they also make seniors feel less thirsty-by 30% to 40%, according to a 2022 study. That means they drink less, sweat less, and risk dehydration faster.
- ACE inhibitors and ARBs (like Benazepril, Losartan): Used for high blood pressure and heart disease, these drugs reduce thirst by about 25%. They also lower blood volume, which makes it harder for the body to circulate blood to the skin for cooling.
- Antipsychotics (like Quetiapine, Clozapine): Often prescribed for dementia or severe anxiety, these interfere with the brain’s thermostat. Studies show they can raise core body temperature by 1.5°F to 2°F even before physical activity.
- Anticholinergics (like Benadryl, Tylenol PM): Found in many sleep aids and allergy meds, these drugs cut sweating by 35% to 50%. Without sweat, the body can’t cool down.
- Some antibiotics and antifungals: Certain types make skin react to sunlight like it’s on fire. Sunburn risk can jump 4 to 6 times higher, and that’s not just about pain-it’s about heat stress.
Worst of all, these risks multiply when medications are taken together. For example, a senior on both a diuretic and an ACE inhibitor might lose sodium faster than their body can replace it. Sodium levels dropping below 135 mmol/L can lead to confusion, falls, seizures, or even cardiac arrest. The CDC found that 22% of heat-related hospitalizations in seniors involve this kind of dangerous combo.
What You Can Do: A Practical Medication Review
Preventing heat-related problems starts with knowing what’s in your medicine cabinet. Don’t wait for a heat wave to act. Before summer hits, sit down with your doctor or pharmacist and ask:
- Which of my medications make me more sensitive to heat?
- Do I need to adjust my dose or timing on hot days?
- Should I temporarily pause any meds that aren’t critical during extreme heat?
- Do I need to change how I manage fluid intake?
Research from Johns Hopkins shows that seniors who had a structured medication review before summer had 37% fewer heat-related ER visits. That’s not a small number-it’s life-changing. Your doctor might suggest switching to a different blood pressure med that doesn’t affect thirst, or reducing the diuretic dose on days when the heat index is above 90°F. Never change your meds on your own, but do ask about alternatives.
Also, check for hidden anticholinergics. Many over-the-counter sleep aids and cold meds contain diphenhydramine or chlorpheniramine. These aren’t labeled as "dangerous in heat," but they are. Swap them for non-drowsy options like loratadine or melatonin if you need help sleeping.
Hydration That Actually Works
Drinking water isn’t enough if your body isn’t holding onto the right balance of salts and minerals. Seniors on diuretics need more than just H2O-they need electrolytes.
The American Geriatrics Society recommends drinking 8 to 10 eight-ounce glasses of fluid daily during hot weather. But if you’re on fluid restrictions (common for heart failure patients), talk to your doctor first. About 43% of those on fluid limits develop dangerous electrolyte imbalances during heat waves.
For those taking diuretics, choose drinks with 120-150 mg of sodium per 8 oz. Look for sports drinks labeled "low sugar" or electrolyte tablets you can dissolve in water. Avoid caffeine and alcohol. Both act as diuretics themselves, increasing urine output by 40% to 60%. That’s like pouring water out of a bucket with a hole in it while trying to fill it.
Set phone alarms every 2 hours to drink a glass of water-even if you’re not thirsty. Thirst is one of the first things that fades with age and medication use. By the time you feel thirsty, you’re already dehydrated.
Staying Cool Without Air Conditioning
Not every senior has air conditioning. But staying cool doesn’t require a fancy system.
The CDC says indoor temperatures should stay below 78°F (25.6°C) during heat waves. If you don’t have AC, use fans to move air around, especially at night. Close blinds and curtains during the day to block heat. Open windows at night if the outside air is cooler. Place a bowl of ice in front of a fan for a DIY air cooler.
Wear loose, light-colored clothing made from cotton or linen. These fabrics breathe better than synthetics and can make you feel 5°F to 7°F cooler. Avoid dark colors-they absorb heat. Use a wide-brimmed hat and UV-blocking sunglasses when outside.
Sunscreen is non-negotiable. Many medications make skin burn faster. Use broad-spectrum SPF 15 or higher, and reapply every 2 hours-or after sweating. The FDA says some drugs increase sunburn risk by 400% to 600%. That’s not a typo. One bad burn can trigger heat stress.
What Caregivers and Family Should Watch For
If you’re helping an older loved one, your role is critical. Heat symptoms in seniors don’t always look like textbook heat exhaustion. They might seem confused, quiet, or off-not sweaty or flushed.
Watch for these early signs:
- Unusual confusion or forgetfulness
- Reduced speech or slurred words
- Loss of appetite or nausea
- Dizziness when standing up
- Dark yellow urine or infrequent urination
Research from UCLA found that caregivers who checked for these subtle changes reduced progression to heat stroke by 62%. Make daily check-ins part of your routine. Ask: "How are you feeling?" not just "Are you okay?"
Plan outings for early morning or evening. Avoid being outside between 10 a.m. and 4 p.m., when heat peaks. Go to the library, mall, or community center instead. Many senior centers open their doors during heat alerts.
Some communities have "I’m OK" programs where volunteers call seniors daily during heat waves. If you don’t have access to one, set up a simple text or phone chain with neighbors or friends to check in.
When to Call 911: Heat Stroke Is an Emergency
Heat exhaustion can turn into heat stroke in as little as 2 to 4 hours. And heat stroke kills. The CDC says 65% of untreated heat exhaustion cases become heat stroke.
Heat stroke looks like this:
- Body temperature above 103°F (39.4°C)
- Hot, red, dry, or damp skin (no sweating)
- Rapid, strong pulse
- Confusion, slurred speech, or unconsciousness
If you see any of these, call 911 immediately. Don’t wait. While waiting for help:
- Move the person to a cool, shady spot
- Remove excess clothing
- Apply cool, wet cloths to the neck, armpits, and groin
- Give cool water if they’re awake and able to swallow
- Do NOT give fever reducers like acetaminophen-they don’t work on heat stroke
Heat stroke doesn’t always come with a warning. That’s why prevention is everything.
New Tools to Help You Stay Safe
There’s new tech making it easier to track risk. The CDC launched the Heat and Medication Risk Assessment Tool (HM-RAT) in June 2023. You can enter your medications and zip code, and it gives you a personalized risk score based on local weather forecasts.
The National Institute on Aging also partnered with the EPA to create HeatRisk.gov. It’s a free website that combines medication risk data with real-time heat index maps. Over 1.2 million seniors used it during the 2023 summer season.
There’s even a new supplement in clinical trials designed for seniors on multiple meds. Early results show it improves thermoregulation by 28%. It’s not on the market yet, but your doctor might know about it.
Climate change isn’t slowing down. The CDC predicts extreme heat days will increase by 50% by 2050. That means heat-related medication problems will become one of the top five preventable causes of death in seniors. The good news? You don’t need to wait for policy changes to protect yourself or your loved ones. Small, smart steps today can save lives tomorrow.
Can I stop my diuretic during a heat wave to avoid dehydration?
Never stop or change your medication without talking to your doctor. Diuretics are often prescribed for serious conditions like heart failure or high blood pressure. Stopping them suddenly can be dangerous. Instead, ask your doctor if your dose can be temporarily lowered during hot weather or if you can switch to a different type of medication that doesn’t affect thirst as much.
Do all seniors on blood pressure meds need to worry about heat?
Not all. ACE inhibitors, ARBs, and diuretics carry the highest risk. Beta-blockers and calcium channel blockers are generally safer in heat, but they can still reduce blood flow to the skin, making cooling less efficient. It’s not about the condition-it’s about the specific drug. Always check with your pharmacist or doctor.
Is it safe for seniors to use fans during heat waves?
Fans help when the air is cooler than your body, but they’re not enough when temperatures hit 95°F or higher. At that point, fans just blow hot air around. If you rely on a fan, combine it with cool cloths, open windows at night, and a spray bottle of water. If possible, spend part of the day in a cooled public space like a library or mall.
What if my senior loved one refuses to drink more water?
Try making fluids more appealing. Offer ice pops made from 100% fruit juice or electrolyte drinks. Use a straw or a cup with a lid to make drinking easier. Try small sips every 20 minutes instead of large amounts. Also, check if they’re avoiding fluids because they fear frequent bathroom trips. Talk to their doctor about adjusting diuretic timing-maybe give it in the morning only, so they can sleep through the night without needing to go.
Are there any foods that help with heat safety?
Yes. Water-rich foods like watermelon, cucumbers, oranges, strawberries, and yogurt can help with hydration. Soups and broths provide both fluids and sodium. Avoid salty snacks like chips or processed foods-they make your body hold onto water unevenly. A balanced diet with fruits, vegetables, and lean proteins supports better fluid balance overall.

Niamh Trihy
January 30, 2026 AT 20:46I'm a geriatric nurse in Dublin, and this post is spot-on. I've seen too many seniors end up in the ER because they stopped their diuretic 'just for a few days' during a heatwave. The body doesn't bounce back like it used to. Always consult your pharmacist - they know the drug interactions better than most doctors do. And yes, electrolyte drinks with sodium are crucial. Water alone is like trying to fill a leaky bucket.
Jason Xin
January 31, 2026 AT 08:40Wow. So let me get this straight - the government wants us to trust a website called HeatRisk.gov that somehow knows what meds we’re on? Cool. Next they’ll be scanning our pill bottles with drones. I’ve got my grandma on Benadryl PM and she’s fine. She’s 84, eats pie for breakfast, and still walks to the corner store. Maybe the real problem is we’ve turned normal aging into a medical emergency.
Kathleen Riley
February 2, 2026 AT 04:43It is a matter of profound philosophical concern that the human organism, in its senescent state, has become increasingly vulnerable to the thermodynamic exigencies of anthropogenic climate change, compounded by the pharmacological interventions ostensibly designed to preserve homeostasis. The confluence of pharmacological inhibition of thermoregulatory mechanisms with rising ambient temperatures constitutes, in effect, a bioethical paradox: we medicate to sustain life, yet those very medications render the body incapable of sustaining itself under natural environmental stressors. One is left to contemplate whether medical progress has outpaced biological resilience.
Beth Cooper
February 3, 2026 AT 18:33Okay but have you heard about the hidden agenda? The CDC and Big Pharma are pushing this heat-meds scare so seniors will buy more 'electrolyte tablets' and stop using their $2 Benadryl. Meanwhile, the real cause of heat deaths? Air conditioning being outlawed in retirement homes to save 'energy.' Also, did you know the sun is actually a hologram projected by the government to control our circadian rhythms? My cousin’s neighbor’s dog got heatstroke last year - and guess what? He was on a diuretic. Coincidence? I think not.