How to Read Contraindications and Warnings on Drug Labels: A Clear Guide for Patients

Medication Safety Checker
Answer the questions below to identify potential medication risks. This tool is for educational purposes only and should not replace professional medical advice.
Remember: The FDA requires prescription drug labels to include boxed warnings for serious risks. Contraindications mean "never take," while warnings mean "be careful." Always discuss with your doctor or pharmacist.
Select any conditions you have:
Select medications you are taking:
Every time you pick up a new prescription or grab a bottle of over-the-counter medicine, you’re holding a legal document that could save your life-or hurt you if you don’t understand it. The drug label isn’t just fine print. It’s your front-line defense against dangerous side effects, deadly interactions, and avoidable mistakes. Yet most people skim it like a manual for a toaster they never use. That’s dangerous. Here’s how to actually read it.
Start with the Boxed Warning
If there’s one thing you must read first, it’s the Boxed Warning. Also called a Black Box Warning, this is the FDA’s strongest safety alert. It’s printed in bold, surrounded by a thick black border, and appears at the very top of the prescription label. This isn’t a suggestion. It’s a red flag for risks that can cause death or serious injury.For example, the antidepressant bupropion carries a boxed warning for increased suicidal thoughts in young adults under 25. Warfarin, a blood thinner, warns of major or fatal bleeding. These aren’t rare outcomes. The FDA requires them only when evidence shows a clear, serious threat. If your drug has one, don’t ignore it. Talk to your doctor about why they still think it’s right for you.
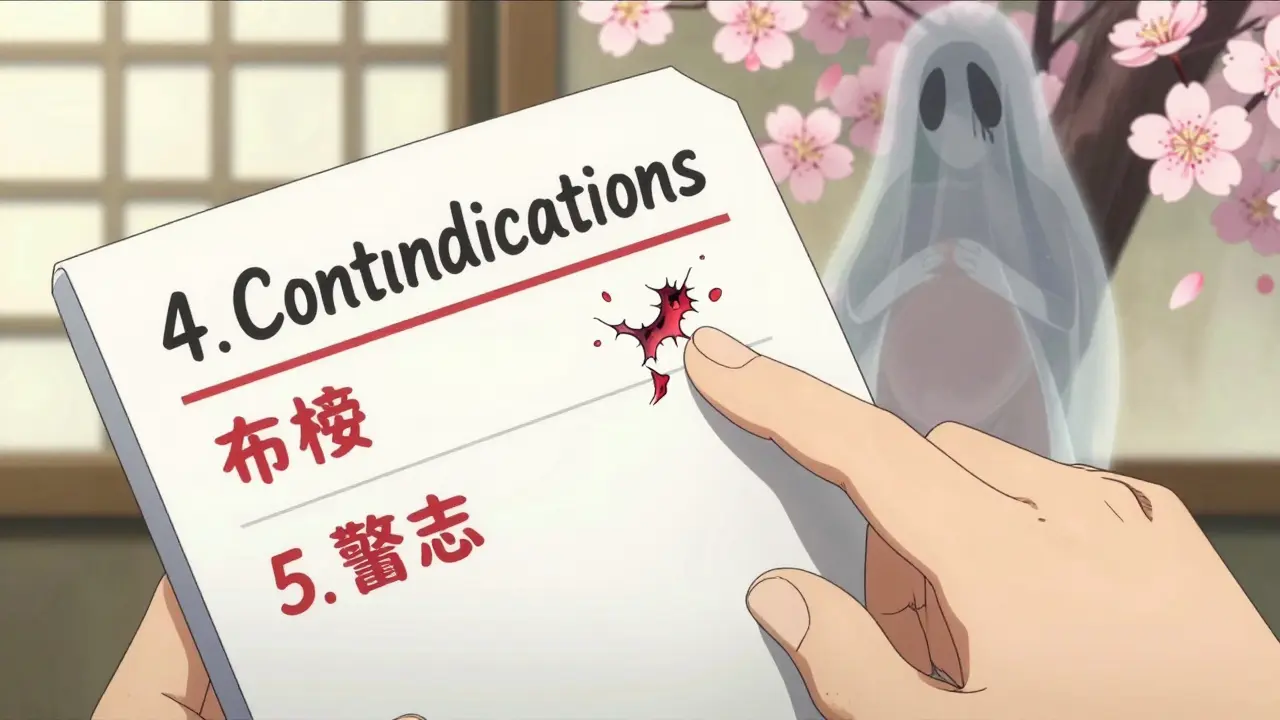
Section 4: Contraindications - When Not to Take It
This is the section that says: “Do not use this drug if…”. It’s labeled as Section 4 in prescription labels. Contraindications mean: never take this drug under these conditions. There’s no safe way around it.Common examples:
- Severe liver disease - drugs like statins or certain antibiotics can cause liver failure in people with existing damage.
- Allergy to any ingredient - even a dye or filler can trigger anaphylaxis.
- Active bleeding - anticoagulants like rivaroxaban are absolutely forbidden if you’re currently bleeding internally.
- Pregnancy - some drugs cause birth defects. The label will say “Pregnancy Category X” or list specific risks.
Don’t assume your doctor already checked this. Sometimes, a condition you forgot to mention - like a past stroke or kidney transplant - could be a hidden contraindication. Always double-check.
Section 5: Warnings and Precautions - When to Be Careful
This is where things get messy. Unlike contraindications, warnings aren’t “never.” They’re “be careful.” These are risks that might happen - and you need to monitor for them.For example, the arthritis drug adalimumab (Humira) warns of serious infections like tuberculosis or sepsis. It doesn’t say “don’t take it.” It says: “We’ve seen this happen in 3.5 out of every 100 patients per year. Watch for fever, chills, or cough. Tell your doctor immediately if you feel sick.”
Here’s how to read this section:
- Look for phrases like “may increase risk,” “use with caution,” or “monitor for.”
- Check if it mentions specific groups - older adults, people with diabetes, those on other meds.
- Find out what you should do if something happens. Does it say to stop the drug? Get blood tests? Call your doctor right away?
Don’t just read the scary parts. Read the solutions too. A warning isn’t a death sentence - it’s a checklist.
OTC Labels Are Different - But Just as Important
Over-the-counter drugs like ibuprofen or allergy pills don’t use the same 16-section format. Instead, they follow the FDA’s Drug Facts label. Here’s how to decode it:- “Do not use” = contraindication. If you have asthma and the label says “do not use if you have asthma,” don’t take it.
- “Ask a doctor before use if” = precaution. This means your condition might make it risky. Maybe you have high blood pressure, or you’re pregnant. Don’t guess - ask.
- “Stop use and ask a doctor if” = red flag during use. If you get a rash, dizziness, or stomach pain after starting, stop immediately.
A 2022 FDA study found only 52% of people could correctly identify absolute contraindications on OTC labels. That’s almost half. You don’t want to be in that group.
What About Drug Interactions?
Many people think drug interactions are listed in a separate section. They’re not. They’re buried in Warnings and Precautions - often under “Drug Interactions” or “Use with Other Medications.”For example, the blood thinner apixaban warns: “Avoid concurrent use with strong CYP3A4/P-gp inhibitors like ketoconazole or clarithromycin.” That’s medical jargon. In plain terms: don’t take this with certain antibiotics or antifungals. Your pharmacist can help translate this.
Here’s a trick: write down every medication you take - even supplements like St. John’s wort, fish oil, or magnesium. Bring that list to every appointment. Many dangerous interactions happen because patients forget they’re taking something “natural.”
Relative vs. Absolute Contraindications - Know the Difference
Not all “don’ts” are equal. An absolute contraindication means no exceptions. Example: never take methotrexate if you’re pregnant.A relative contraindication means: “It’s risky, but we might still use it if benefits outweigh risks.” Example: taking a beta-blocker if you have mild asthma. Your doctor might lower the dose, monitor you closely, or choose a different drug.
Most confusion comes from this gray zone. If your label says “use with caution in patients with kidney disease,” ask: “How bad is my kidney disease? Is this safe for me?” Don’t assume your doctor already figured it out.

Why This Matters: Real Stories, Real Risks
One Reddit user shared how their cardiologist prescribed amiodarone - a heart drug with a boxed warning for lung damage - despite mild lung disease. The pharmacist almost refused to fill it because they didn’t read the label closely. The label said “contraindicated in severe pulmonary disease.” Mild was okay. But only if the doctor knew the difference.The FDA received over 12,000 consumer questions about drug warnings in 2022. Nearly half were about unclear interactions. People didn’t know if it was safe to take their painkiller with their tea, their vitamin, or their neighbor’s leftover antibiotic.
These aren’t hypothetical risks. The Institute of Medicine estimates 1.3 million injuries each year in the U.S. come from poor labeling - not from bad doctors or bad pills. From bad understanding.
What You Can Do Today
You don’t need to be a doctor to read a drug label. You just need to know where to look.- Always read the Boxed Warning first.
- Find Section 4: Contraindications. Ask: “Is this me?”
- Read Section 5: Warnings. Ask: “What should I watch for? What do I do if it happens?”
- For OTC drugs: scan “Do not use,” “Ask a doctor,” and “Stop use.”
- Bring a list of all your meds - including supplements - to every appointment.
- If something sounds confusing, ask: “Can you explain this in plain English?”
There’s no shame in asking. The FDA’s own data shows even doctors miss key details. In one study, only 42% of physicians correctly identified relative contraindications. You’re not alone.
What’s Changing - And Why It Matters
The FDA is trying to fix this. In 2024, new drug labels must include a “Highlights” section that summarizes the most critical warnings in plain language. Some companies are starting to use color-coded risk levels and numbers - like “increases heart attack risk by 1.8 times in people over 65.” That’s better than vague phrases like “may cause heart problems.”But until then, you’re still the last line of defense. Don’t let the label be a mystery. Treat it like a safety manual for your body. Because it is.
What’s the difference between a contraindication and a warning?
A contraindication means you should never take the drug under certain conditions - like having a severe allergy or active bleeding. It’s a hard stop. A warning means the drug can be used, but with caution. You might need extra monitoring, a lower dose, or to watch for side effects. Think of contraindications as red lights and warnings as yellow lights.
Can I still take a drug if it has a boxed warning?
Yes - but only if your doctor believes the benefits outweigh the risks. Boxed warnings are serious, but they don’t mean the drug is banned. For example, many people take antidepressants with boxed warnings for suicidal thoughts because the alternative - untreated depression - is more dangerous. Your doctor should explain why they’re still prescribing it, and you should ask: “What signs should I watch for? What if I notice them?”
Do I need to read the label every time I refill a prescription?
Yes. Drug labels change. New risks are discovered after a drug is on the market. A warning you didn’t see last year might be added this year. Even if you’ve taken the same pill for years, always check the label when you get a new bottle. The FDA requires manufacturers to update labels within 30 days of new safety data.
What if I don’t understand the medical terms on the label?
Ask your pharmacist. They’re trained to translate medical jargon into plain language. You can also call the drug manufacturer’s patient information line - it’s listed on the label. Don’t guess. Misunderstanding “severe renal impairment” as “a little kidney trouble” could be deadly. It’s not your fault if the language is confusing - it’s the system’s job to make it clear.
Are natural supplements safe to take with prescription drugs?
Not always. Many people assume “natural” means “safe,” but that’s false. St. John’s wort can make birth control, antidepressants, and blood thinners stop working. Garlic and ginkgo can increase bleeding risk with anticoagulants. Fish oil can interact with blood pressure meds. Always list every supplement on your medication list - even if you think it’s harmless.
Why do some drugs have warnings for conditions I don’t have?
Because drug labels are written for everyone who might take the drug - not just you. If a drug causes liver damage in 1 out of 1,000 people with hepatitis, the warning will say “avoid in liver disease,” even if you’re perfectly healthy. The label doesn’t know your history. It’s designed to cover all possible cases. That’s why you need to read it with your own situation in mind.
If you’re ever unsure - pause. Don’t take the pill. Call your doctor or pharmacist. One minute of asking questions could prevent a hospital visit. Your body doesn’t care how smart the label looks. It only cares if you understood it.

Sue Stone
January 24, 2026 AT 11:00Finally someone gets it. I used to skip the label like it was a Terms of Service I’d never read. Then my cousin ended up in the ER because she took ibuprofen with her blood thinner. Don’t be her.
dana torgersen
January 25, 2026 AT 19:22so like… the boxed warning? it’s not just for show?? i mean… like… wow. i thought it was just there to scare people into buying the brand name version… not that it’s actually… like… life or death??
Stacy Thomes
January 26, 2026 AT 01:14THIS. I’ve been telling my mom for years to read the tiny print. She thinks if the pharmacy gave it to her, it’s automatically safe. Nope. Your body is not a vending machine.
Susannah Green
January 27, 2026 AT 05:11Don’t forget the ‘Stop use and ask a doctor’ line on OTC meds! I ignored it when my knee swelled after taking naproxen for a week. Turned out I had a hidden ulcer. Now I check every bottle like it’s a bomb defusal manual.
Vanessa Barber
January 29, 2026 AT 02:06Yeah right, like anyone reads these labels. My aunt took melatonin with her antidepressant because ‘it’s natural’ and ended up in a coma. The label didn’t stop her. The ER did.
Dawson Taylor
January 29, 2026 AT 12:11The systemic failure here isn’t patient ignorance-it’s the assumption that legal language equates to understood meaning. The FDA mandates clarity, yet the vocabulary remains alien to the layperson. The onus is misplaced. We don’t need more warnings. We need translation.
Kerry Evans
January 29, 2026 AT 14:24People think they’re ‘too smart’ to need this. I’ve seen PhDs take statins while eating grapefruit and say ‘I didn’t know it interacted.’ You don’t need a degree to read. You need humility.
Andrew Smirnykh
January 30, 2026 AT 04:43In Nigeria, we often rely on pharmacists because labels are printed in English but spoken in Pidgin. The real issue isn’t reading-it’s access to someone who can explain. Maybe this guide should be turned into audio for low-literacy communities.
Janet King
January 31, 2026 AT 17:01Always bring your medication list to appointments. Include herbal supplements, vitamins, and even over-the-counter sleep aids. Many interactions occur because patients omit what they consider ‘not medicine.’ The pharmacist is your best ally.
Laura Rice
February 1, 2026 AT 04:52I used to roll my eyes at ‘read the label’… until I almost gave my grandma the wrong dose of her thyroid med because I assumed the pill looked the same as last month. Turns out, the manufacturer changed the filler. The label said so. I didn’t look. Now I take a picture of every bottle. No shame.
Kerry Moore
February 2, 2026 AT 04:44Relative contraindications require nuanced clinical judgment. The physician’s responsibility is not merely to prescribe, but to contextualize risk. A patient with mild renal impairment may safely receive metformin with appropriate monitoring. The label informs, but the clinician interprets. Both are necessary.
Anna Pryde-Smith
February 3, 2026 AT 09:30MY AUNT DIED BECAUSE SHE IGNORED THE BOXED WARNING ON HER ANTIBIOTIC. SHE THOUGHT IT WAS JUST ‘SCARY WRITING.’ SHE DIDN’T KNOW IT COULD KILL HER LUNGS. NOW I READ EVERY LABEL LIKE MY LIFE DEPENDS ON IT. BECAUSE IT DOES.
charley lopez
February 4, 2026 AT 16:54The pharmacokinetic interplay between CYP3A4 substrates and inhibitors remains underappreciated in primary care. The label’s reference to ‘strong inhibitors’ is insufficient without context of half-life, protein binding, and hepatic clearance profiles. Patients require more than bullet points-they require mechanism.
Oladeji Omobolaji
February 4, 2026 AT 20:25Here in Nigeria, we don’t always get labels in English. Sometimes it’s just a sticker with a picture of a pill and ‘take one.’ My cousin took his dad’s blood pressure med because it looked the same. He ended up in the hospital. We need pictures, symbols, voice notes. Not just words.