How to Talk to Your Doctor About Generic Medications

Many people assume that generic medications are cheaper because they’re less effective. That’s not true. In fact, the generic medications your doctor prescribes contain the exact same active ingredients as the brand-name versions. They work the same way. They just cost a fraction of the price.
Yet, nearly half of patients still hesitate to take them. Why? Because they’ve heard rumors. They’ve seen different shapes, colors, or names on the bottle. They worry about quality. Or worse - they think their doctor is cutting corners. The truth is, the FDA requires generics to meet the same strict standards as brand-name drugs. Every single one. But if you don’t ask the right questions, you’ll never know that.
What exactly makes a drug "generic"?
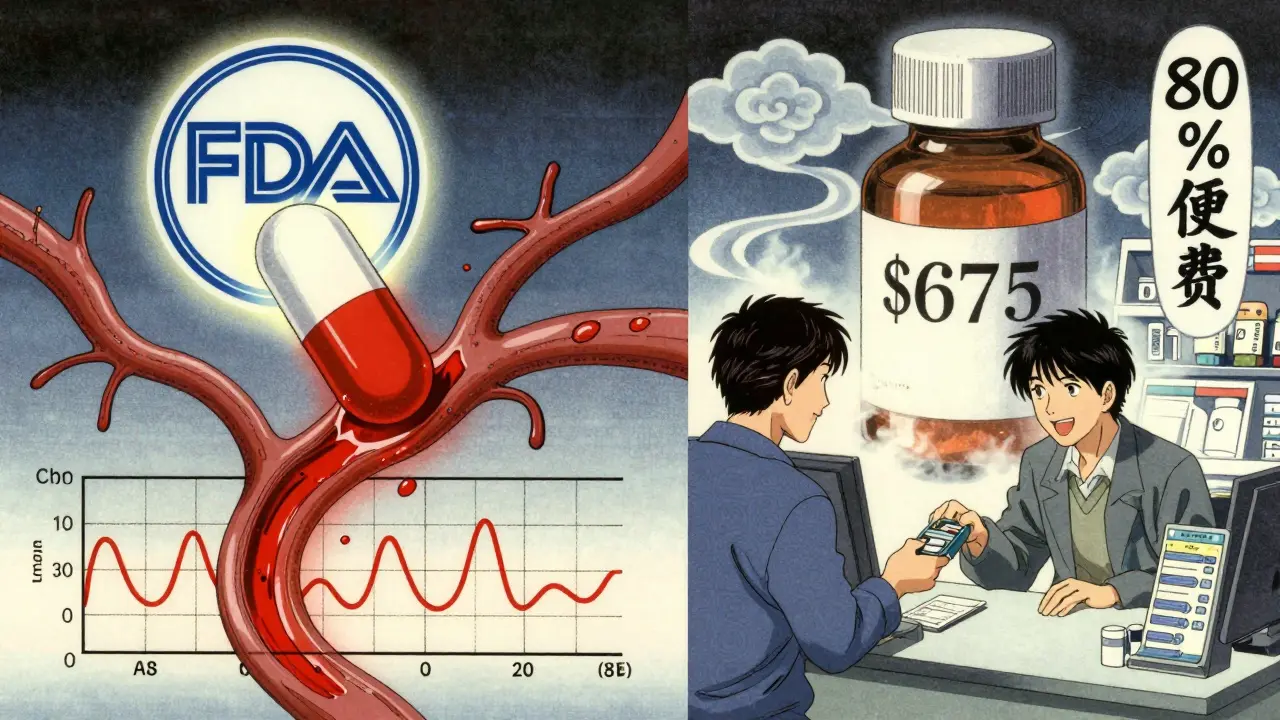
A generic drug isn’t a copy. It’s a copy that’s been proven to work the same. The FDA doesn’t just approve generics based on paperwork. They require manufacturers to prove bioequivalence - meaning the drug gets into your bloodstream at the same rate and in the same amount as the brand-name version. That’s measured using two key numbers: Cmax (how high the drug peaks in your blood) and AUC (how much of the drug your body absorbs over time). Both must fall within 80% to 125% of the brand-name drug’s numbers. That’s not a guess. That’s science.
And it’s not just about the active ingredient. Generics must match the brand in strength, dosage form (pill, injection, capsule), and how you take it (by mouth, under the tongue, etc.). The only differences? The color, shape, flavor, or inactive ingredients like fillers or dyes. These don’t affect how the drug works. They’re just there to make the pill look different or easier to swallow.
Here’s the kicker: the FDA inspects every generic manufacturing plant the same way they inspect brand-name ones. Same rules. Same standards. Same inspections. In 2023, 98.7% of generic facilities passed FDA inspections. That’s higher than the average for brand-name facilities.
Why do generics cost so much less?
Brand-name drugs cost tens of thousands of dollars to develop. Companies spend years running clinical trials, patenting formulas, and marketing. Once the patent expires, other companies can make the same drug - without repeating those expensive steps. That’s why generics cost 80% to 85% less. A typical brand-name prescription might cost $675. The generic? Around $16.
That’s not a coincidence. It’s the whole point of the system. Since 1984, the Hatch-Waxman Act created a legal path for generics to enter the market faster. Today, 90% of all prescriptions in the U.S. are filled with generics. But they only make up 23% of total drug spending. That’s $1.7 trillion saved every year across the country.
And the savings aren’t just for insurance companies. If you’re on Medicare Part D, you could be saving over $5,200 a year just by choosing generics when available. The Inflation Reduction Act is making that even easier - by 2025, many generics will be free at the pharmacy counter.
Do generics really work as well?
Yes. And not just a little better - a lot better.
A 2020 study in JAMA Internal Medicine looked at 47 clinical trials comparing generics and brand-name drugs for heart conditions. The results? No meaningful difference in effectiveness. Zero. The p-value was 0.73 - meaning the chance of a real difference was less than 1 in 4.
And it’s not just heart drugs. Studies on antidepressants, blood pressure meds, diabetes pills, and even thyroid hormones show the same thing. Generics work. In fact, patients who take generics are 8% to 12% more likely to keep taking their medication. Why? Because they can afford it. When people stop taking meds because they’re too expensive, their health gets worse. That leads to more hospital visits, more ER trips, and higher costs overall.
There’s one exception: narrow therapeutic index drugs. These are medications where even tiny changes in blood levels can cause problems - like warfarin, lithium, or levothyroxine. For these, the FDA requires even tighter bioequivalence standards (90% to 110%). And even then, most patients do just fine switching. A small number report feeling different - usually because of inactive ingredients, not the active drug. If that happens, talk to your doctor. But don’t assume it means the generic doesn’t work.
What do patients actually worry about?
When patients are asked why they avoid generics, three reasons come up again and again:
- "Cheaper means worse." - 68% of people believe this, even though it’s not true.
- "The pills are made overseas." - 52% worry about manufacturing quality. But the FDA inspects plants in the U.S., India, China, and everywhere else - the same way.
- "I don’t trust the system." - 47% feel like they’re being sold a second-rate product.
These fears aren’t silly. They’re real. And they cost the healthcare system $290 billion a year in avoidable hospitalizations and emergency care. That’s because when people stop taking their meds, their condition gets worse. And then they end up in the hospital - which costs way more than the drug ever did.
One patient on Reddit said, "I switched to generic metoprolol and felt dizzy for two weeks." But when she talked to her pharmacist, she learned the inactive ingredient changed. She was switched to a different generic version - and the dizziness went away. That’s not a failure of generics. That’s a failure of communication.
How to start the conversation with your doctor
You don’t need to be an expert. You just need to ask the right questions. Here’s how to do it - without sounding confrontational.
Step 1: Ask what you know. Start with, "I’ve heard a lot about generics. What’s your take?" This opens the door. It tells your doctor you’re curious, not skeptical.
Step 2: Listen and share your concerns. Say something like, "I’m worried the generic won’t work the same. Is that possible?" Or, "I’ve seen different pills before - why do they look different?" Your doctor can explain the inactive ingredients. They can show you the FDA’s fact sheet. They can even pull up the bioequivalence data if needed.
Step 3: Ask them to check back. Say, "Can we try the generic? If I feel any difference, I’ll let you know. Then we can switch back." Most doctors will agree. And if you do notice something - like a new rash, nausea, or dizziness - it’s not because the drug doesn’t work. It’s because your body is adjusting to a new filler. That’s fixable.
Doctors who use the "Ask-Tell-Ask" method (ask what you know, tell the facts, ask you to repeat it back) reduce medication errors by 37%. That’s not magic. It’s just good communication.
What to do if you’re still unsure
If you’re still hesitant, ask for the FDA’s Medication Guide. By law, your pharmacist must give you one for certain drugs - whether generic or brand. These guides are written in plain language (5th to 7th grade level) and explain exactly what the drug does, what side effects to watch for, and why generics are safe.
You can also check the FDA’s website for the Orange Book - a public database that lists every approved generic and its brand-name match. You don’t need to be a scientist to use it. Just search by drug name. You’ll see the approval date, the manufacturer, and the bioequivalence data.
And if you’re on a tight budget? Ask your pharmacist. They see this every day. They know which generics are most affordable. They know which ones have the fewest reports of side effects. And they’re trained to explain it clearly.

Real stories from real patients
One man in Ohio switched from brand-name Lipitor to generic atorvastatin. His co-pay dropped from $98 to $4. He didn’t feel any different. His cholesterol stayed stable. He said, "I was scared I’d feel worse. I felt better knowing I saved money without losing protection."
A woman in Texas with high blood pressure was told her generic lisinopril wouldn’t work as well. She asked her doctor for proof. He showed her the JAMA study. She switched. Her BP improved. Her insurance bill dropped by $1,200 a year.
On GoodRx’s 2023 survey of 12,500 people, 79% said they noticed no difference after switching to generics. 68% said they asked for the generic because they couldn’t afford the brand. Not because they were desperate - because they were smart.
When you shouldn’t switch
There are rare cases where switching isn’t recommended. If you’ve been on the same brand for years and it’s working perfectly, and you’ve never had side effects - you don’t need to change. But don’t assume you can’t switch. Talk to your doctor first.
Also, if you’re on a drug with a narrow therapeutic index - like warfarin, levothyroxine, or cyclosporine - stick with the same generic brand if possible. Why? Because even though all generics are safe, your body may respond slightly differently to different fillers. If you switch between generics frequently, your levels might fluctuate. That’s why doctors often prescribe one specific generic for these drugs. It’s not because the others don’t work. It’s to keep your levels steady.
And if you’ve had a bad reaction to a specific generic in the past - tell your doctor. That’s not a reason to avoid all generics. It’s a reason to avoid that specific manufacturer’s version.
What’s next for generics?
The future is getting even better. The FDA is rolling out a new tool called the "Generic Drug Navigator" - a chatbot that answers common questions in plain language. By 2025, more prescriptions will come with QR codes that link to short videos explaining the drug, how to take it, and why the generic is safe.
And the big push? Making generics free. By 2025, Medicare Part D will cover many generics with $0 cost-sharing. That means no co-pay. No deductible. Just walk in, get your pill, and leave.
This isn’t about cutting corners. It’s about making care affordable. Generics aren’t a compromise. They’re the smart choice. And the best part? You already have the power to choose them.
You don’t need to wait for your doctor to bring it up. You don’t need to be afraid to ask. You just need to start the conversation. And if you do - you’ll save money, stay healthier, and take back control of your care.

Ann Romine
January 1, 2026 AT 03:48I used to avoid generics because I thought they were "cheap drugs." Then I switched to generic metoprolol after my pharmacist explained the bioequivalence data. No difference in how I felt-just saved $80 a month. Sometimes the real cost isn’t the pill, it’s the fear we carry around it.
Todd Nickel
January 1, 2026 AT 08:58The FDA’s bioequivalence standards for generics are actually more rigorous than most people realize. The 80–125% confidence interval for Cmax and AUC isn’t arbitrary-it’s statistically derived from pharmacokinetic modeling across hundreds of subjects, and it accounts for inter-individual variability in absorption. What’s more, the 2023 FDA inspection pass rate for generic facilities (98.7%) outpaces brand-name plants, which hover around 96%. This isn’t a loophole-it’s a well-regulated, science-backed system that’s been refined since Hatch-Waxman. The real issue isn’t efficacy; it’s the cultural stigma around cost-saving measures in healthcare, which is oddly classist when you think about it.
Phoebe McKenzie
January 2, 2026 AT 18:12STOP lying to people. Generics are NOT the same. I switched to generic levothyroxine and my TSH went from 2.1 to 7.8 in three weeks. My doctor said "it’s just the filler," but my body knew. The FDA doesn’t test how you FEEL. They test numbers. And if you’re one of the 3% who react to the dye or binder? You’re screwed. This post is dangerous. People die because they’re pressured into switching. Don’t be a pawn for Big Pharma’s cheap replacements.
Kristen Russell
January 4, 2026 AT 11:48My mom’s on generic lisinopril-saved her $1,000/year. No side effects. She’s alive because she could afford it. Don’t let fear cost you your health.
Bryan Anderson
January 5, 2026 AT 15:44Thank you for writing this. I’ve been a pharmacist for 18 years, and I’ve seen patients refuse generics out of fear-only to end up in the ER because they stopped taking their meds. The science is clear. The savings are real. And the FDA’s oversight is thorough. If you’re concerned, ask for the Medication Guide. Read it. Talk to your pharmacist. Knowledge is the antidote to misinformation.
Matthew Hekmatniaz
January 6, 2026 AT 06:05My dad’s from India-he used generics for decades before coming to the U.S. He said, "Back home, we didn’t have a choice. But here, people act like generics are a betrayal." I think it’s about trust, not science. We’ve been sold the idea that expensive = better, even when the data says otherwise. Maybe the real medicine is changing how we think, not just what’s in the pill.
Liam George
January 7, 2026 AT 18:41Let’s be real-this whole generic system is a corporate shell game. The same companies that make brand-name drugs own the generic versions. The FDA’s "independent" inspections? Run by contractors paid by pharma. The "bioequivalence" data? Often submitted by the manufacturer with no third-party verification. And don’t get me started on the Chinese and Indian factories-no transparency, no accountability. You think your $16 pill is safe? You’re just trusting a system designed to maximize profit, not patient outcomes. Wake up.
sharad vyas
January 8, 2026 AT 10:02In India, generics are the only option. We don’t have money for brand names. But we also don’t have the fear you have here. The medicine works. The body knows. Maybe the problem is not the pill-but the story we tell ourselves about it.
Dusty Weeks
January 9, 2026 AT 08:10generic = bad 😡 i got a rash from one. i hate this system. 🤬💊