How to Time Your Medications to Avoid Dangerous Drug Interactions

Every year, tens of thousands of people end up in the hospital not because their medication stopped working, but because they took it at the wrong time. It’s not about taking too much or too little-it’s about when you take it. If you’re on more than a few medications, especially if you’re over 65, the timing between pills can make the difference between staying healthy and ending up in the ER.
Why Timing Matters More Than You Think
Most people think drug interactions mean one pill cancels out another. That’s not always true. Sometimes, the problem isn’t the drugs themselves-it’s how close together you take them. This is called a time-dependent drug interaction (TDDI). It happens when one drug blocks another from being absorbed, or changes how fast your body processes it. And the fix? Simple: wait a few hours. For example, if you take an antacid like Tums or Maalox with ciprofloxacin (a common antibiotic), your body absorbs up to 90% less of the antibiotic. That means the infection might not clear-and could get worse. But if you wait two hours between the antacid and the antibiotic, the antibiotic works just fine. Same thing with levothyroxine, the thyroid medication. If you take it with iron, calcium, or even coffee, absorption drops by half. Wait four hours, and your thyroid levels stay stable. The FDA says about 20-30% of all documented drug interactions can be avoided just by changing the time you take your pills. That’s not a small number. It’s a major safety tool that most people never learn about.Common Medications That Need Space
Not all drugs play nice together-and some need serious distance. Here are the most common ones you need to time carefully:- Levothyroxine (for hypothyroidism): Must be taken on an empty stomach, at least 4 hours before or after iron, calcium, magnesium, aluminum (found in antacids), or soy products. Even your morning coffee can interfere.
- Fluoroquinolone antibiotics (ciprofloxacin, levofloxacin): Don’t take within 2 hours of antacids, multivitamins, or dairy products. Calcium binds to these antibiotics and stops them from working.
- Bisphosphonates (alendronate, risedronate for osteoporosis): Must be taken with a full glass of water, first thing in the morning, and you must wait 30 minutes before eating, drinking, or taking anything else. Otherwise, less than 1% gets absorbed.
- Tetracycline antibiotics (doxycycline, minocycline): Avoid calcium, iron, zinc, and dairy for 2-3 hours before and after. These minerals lock onto the antibiotic like glue.
- Proton pump inhibitors (omeprazole, esomeprazole): If you’re also taking iron or vitamin B12, space them out by at least 2 hours. These drugs reduce stomach acid, which your body needs to absorb certain nutrients.
What Timing Won’t Fix
Not every interaction can be solved by waiting. Some problems happen inside your liver, not your stomach. If two drugs compete for the same enzyme-like warfarin and metronidazole-timing won’t help. Metronidazole blocks the enzyme that breaks down warfarin, so warfarin builds up in your blood. That raises your risk of dangerous bleeding. No matter how far apart you space them, the risk stays high. In cases like this, you need a different solution: either lower the dose of one drug, switch to a different medication, or get more frequent blood tests to monitor your levels. Timing only works when the issue is absorption or stomach chemistry-not metabolism.Why Doctors Don’t Always Tell You
You might be surprised to learn that most prescribing doctors don’t routinely check timing between pills. A 1996 JAMA study found that nearly all drug interaction research ignored timing as a variable. Even today, many electronic prescribing systems flag interactions but don’t suggest how to space them out. Nurses and pharmacists often fill in the gaps, but if you’re seeing multiple doctors or getting prescriptions from different pharmacies, the information gets lost. A 2023 Medscape survey showed that 78% of primary care doctors find managing timing for patients on 5+ medications “moderately to severely difficult.” It’s not that they don’t care-it’s that the system doesn’t make it easy. That’s why you need to be your own advocate.How to Get It Right: A Simple 3-Step Plan
You don’t need to memorize every interaction. Here’s how to handle it step by step:- Make a full list of everything you take. Include prescription drugs, over-the-counter meds, vitamins, and supplements. Write down the dose and how often you take it.
- Check for known timing conflicts. Use trusted sources like Lexicomp, Micromedex, or the FDA’s drug interaction database. Look for any drugs that say “take 2 hours before or after” or “avoid with calcium/iron.”
- Build a daily schedule. Group your pills by when they need to be taken. For example:
- 7:00 AM: Levothyroxine (on empty stomach)
- 7:30 AM: Breakfast
- 10:00 AM: Calcium supplement
- 12:00 PM: Antibiotic
- 2:00 PM: Antacid
- 8:00 PM: Blood pressure med
Tools That Actually Help
If you’re overwhelmed, tech can help. Apps like Medisafe, MyTherapy, or even Apple Health can send you alerts when it’s time to take a pill-and remind you to wait before the next one. A 2021 trial with over 1,200 patients showed that using timed alerts improved adherence by 57%. That’s huge. Some hospitals now use AI-powered systems that adjust timing recommendations based on your kidney function, age, or even what you ate that day. Epic’s 2023 update cuts false alerts by 38% by personalizing timing rules. You might not have access to that yet-but you can still use free apps to get the same benefit.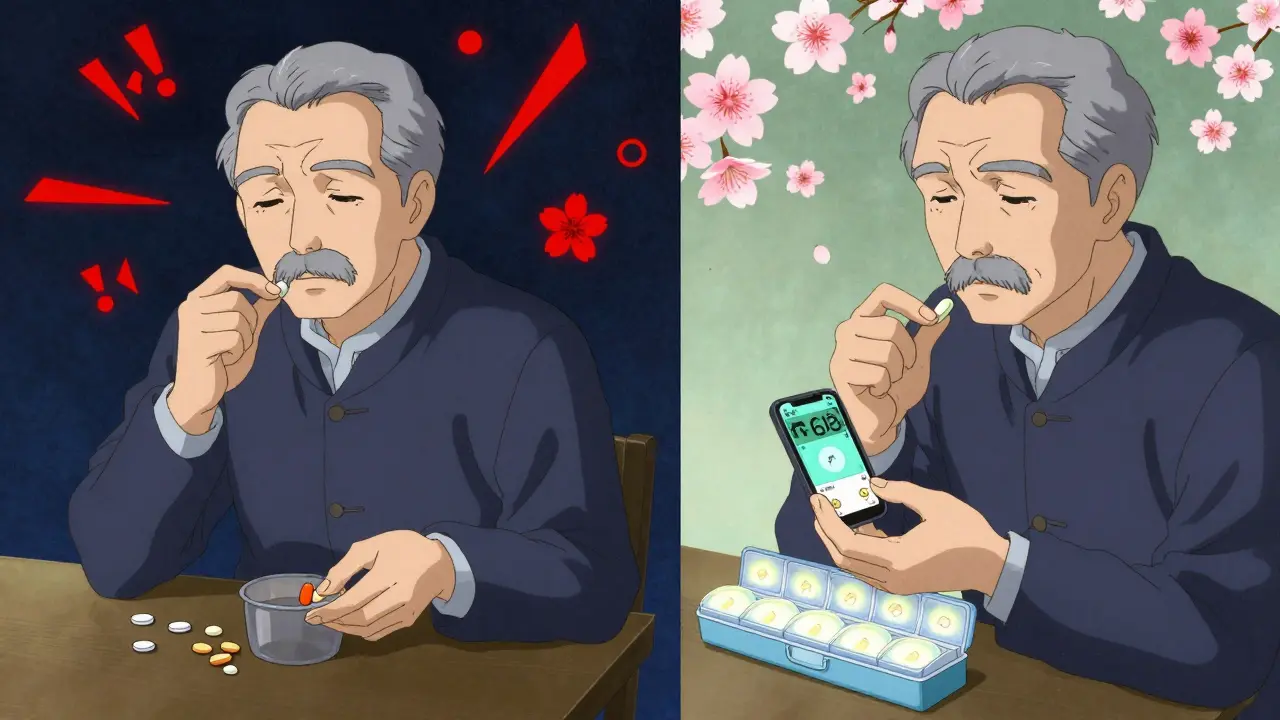
What Happens When You Get It Wrong
Skipping the right timing doesn’t always cause immediate harm. Sometimes, it’s subtle: your thyroid levels drift, your infection lingers, your bones keep weakening. But over time, these small failures add up. In Europe, improper timing accounts for 18% of preventable adverse drug events. In the U.S., the CDC says older adults on five or more medications are three times more likely to have a time-dependent interaction than younger people. One pharmacist in California tracked iron deficiency in elderly patients on levothyroxine and calcium. After introducing a simple 4-hour spacing rule and giving out pill organizers, iron deficiency cases dropped by 32% in 18 months. That’s not luck-it’s smart timing.What to Do If You’re Confused
If you’re unsure whether your meds need spacing, don’t guess. Ask your pharmacist. They’re trained to spot these issues. Bring your pill bottles or a list of everything you take. Say: “I want to make sure I’m taking these at the right times to avoid interactions.” Most pharmacists will review your list for free. If you’re seeing multiple doctors, ask one of them to do a full medication reconciliation. That’s when they review everything you’re on and remove duplicates or conflicts. Medicare now covers this for patients on 5+ medications.Bottom Line: Timing Is a Tool, Not a Trick
You don’t have to stop taking your meds. You don’t have to switch to something else. Sometimes, all you need is a little space between pills. It’s not complicated. It’s not expensive. And it’s one of the most effective ways to stay safe on multiple medications. Start today. Write down your pills. Check one interaction. Space them out. Use an app or a pill box. Talk to your pharmacist. Small changes like this prevent hospital visits, reduce side effects, and help your meds work the way they’re supposed to.Can I take my vitamins with my morning medication?
It depends. Multivitamins often contain calcium, iron, or magnesium-which can block absorption of thyroid meds, antibiotics, and bisphosphonates. If you take levothyroxine, wait 4 hours after your vitamin. If you take ciprofloxacin, wait 2 hours. Always check the label or ask your pharmacist. Better yet, take your vitamins with dinner instead of breakfast.
What if I forget to space my pills and take them together?
Don’t panic. Skip the next dose if it’s close to the time you’re supposed to take the next one. For example, if you took your antibiotic with an antacid by accident, don’t double up later. Just wait until your next scheduled time. Taking extra doses can cause side effects. Going one day without full absorption is usually safe-missing multiple days isn’t. Talk to your doctor if this happens often.
Do I need to time my supplements the same way as prescriptions?
Yes. Supplements like calcium, iron, magnesium, and even herbal products like St. John’s Wort can interfere with prescription drugs. Many people assume “natural” means safe, but that’s not true. Iron and thyroid meds? 4-hour gap. Calcium and antibiotics? 2-hour gap. Treat supplements like medications-they can have real effects on your body.
Can I use a pill organizer to help with timing?
Yes, and it’s one of the best tools you can use. Choose one with separate compartments for morning, afternoon, and evening. Some even have alarms. Studies show they reduce timing errors by 43%. But don’t just fill it all at once. If your meds need different spacing, you may need multiple organizers or a digital reminder system. For example, if you take levothyroxine at 7 AM and calcium at 10 AM, you can’t put them in the same morning slot.
Why does coffee interfere with some medications?
Coffee doesn’t directly interact with most drugs, but it can affect stomach acid and gut movement. For thyroid meds like levothyroxine, drinking coffee within 30-60 minutes of taking the pill can reduce absorption by up to 55%. The same goes for some antibiotics and bisphosphonates. Wait at least an hour after taking your medication before drinking coffee-or take your meds at night if you’re a morning coffee drinker.
Is timing medication safe for elderly patients?
Yes-especially for them. Older adults often take 5-10 medications daily, making timing issues more common and more dangerous. Studies show that with proper education and tools like pill organizers or smartphone alerts, adherence to timing rules improves dramatically. The key is simplifying the schedule. If your regimen is too complex, ask your doctor or pharmacist to review it. Sometimes, switching to once-daily versions or combining pills can reduce the need for spacing.
What if my doctor says timing doesn’t matter?
Get a second opinion. While some interactions are purely metabolic and can’t be timed, many-especially those involving absorption-are well-documented. The FDA, CDC, and American Society of Health-System Pharmacists all recognize timing as a valid strategy. Ask your doctor to check Lexicomp or another trusted drug interaction database. If they’re unsure, ask them to consult a pharmacist. Your safety matters more than convenience.

Neil Thorogood
January 25, 2026 AT 14:00So let me get this straight-I’ve been swallowing my thyroid pill with my coffee like it’s a shot of espresso and now I’m basically a walking zombie? 🤯 I feel like I’ve been playing Russian roulette with my endocrine system. Time to buy a pill organizer and a new life. #ThyroidWarrior #CoffeeIsTheEnemy
Jessica Knuteson
January 27, 2026 AT 04:57Timing is a social construct. The body doesn’t care about your calendar. If the drug works, it works. If it doesn’t, you’re either broken or the system is. Stop overcomplicating medicine with time zones and pill boxes. The real issue is pharmaceutical capitalism.
Robin Van Emous
January 29, 2026 AT 03:46I just want to say thank you for writing this. My mom is 72 and takes 8 different pills every day. She was confused, tired, and always feeling off. We sat down, made a chart, and started spacing things out. Her energy is better. Her lab numbers improved. It’s not magic-it’s just paying attention. Everyone deserves to know this.
Pharmacists are heroes. Don’t be shy to ask them. They’re not paid enough to do this, but they still do it. 🙏
Angie Thompson
January 29, 2026 AT 22:00OMG I JUST REALIZED I’VE BEEN TAKING MY CALCIUM WITH MY ANTIBIOTIC LIKE A MANIAC 😱 I thought supplements were just ‘bonus health’-turns out they’re basically drug saboteurs! 🚨 I’m switching my vitamins to bedtime now. Also, I downloaded Medisafe and it just told me to wait 2 hours before my Tums. I’m crying. This is life-changing. Thank you for not making this sound like a textbook!! 💪💊
Geoff Miskinis
January 30, 2026 AT 21:10It’s amusing how the American healthcare system has reduced pharmacology to a scheduling problem. The real issue is polypharmacy in an aging population with no coordinated care. You can time your pills all day, but if you’re on ten medications because your GP doesn’t know how to deprescribe, you’re just rearranging deck chairs on the Titanic. This article is a Band-Aid on a hemorrhage.
Betty Bomber
January 31, 2026 AT 05:22My grandma used to say, ‘If it ain’t broke, don’t fix it.’ But then she started taking levothyroxine and calcium together and ended up in the ER with a heart flutter. Now she uses a pill box with alarms. She says it’s the only thing keeping her from turning into a zombie. So… yeah. Do the thing.
Mohammed Rizvi
February 1, 2026 AT 11:11Man, I used to think ‘natural’ meant harmless. Then I started taking St. John’s Wort with my blood pressure med and nearly passed out. Turns out ‘herbal’ doesn’t mean ‘safe.’ I now treat every supplement like it’s a loaded gun. And I don’t even take coffee before noon anymore. Small changes, big results. Respect the timing.
eric fert
February 3, 2026 AT 05:14Let’s be real-this whole timing thing is just another way for Big Pharma to sell you more products. Pill organizers? Apps? Alarms? You’re being manipulated into believing that your body can’t handle a few overlapping meds. The truth? Most of these ‘interactions’ are statistically insignificant in real-world use. The FDA and CDC are terrified of admitting that we’ve overmedicated an entire generation. And now they want you to spend your life micro-scheduling every pill like it’s a NASA launch. Wake up. Your body is not a chemistry lab. It’s a living, breathing, adaptive organism. If you’re taking five meds, maybe the real problem is that you’re being treated for symptoms instead of causes. And if you’re over 65 and on ten drugs? You’re not a patient-you’re a walking clinical trial. This article is corporate propaganda dressed up as ‘health advice.’