Low-GI Diet: How Glycemic Index Affects Weight Control

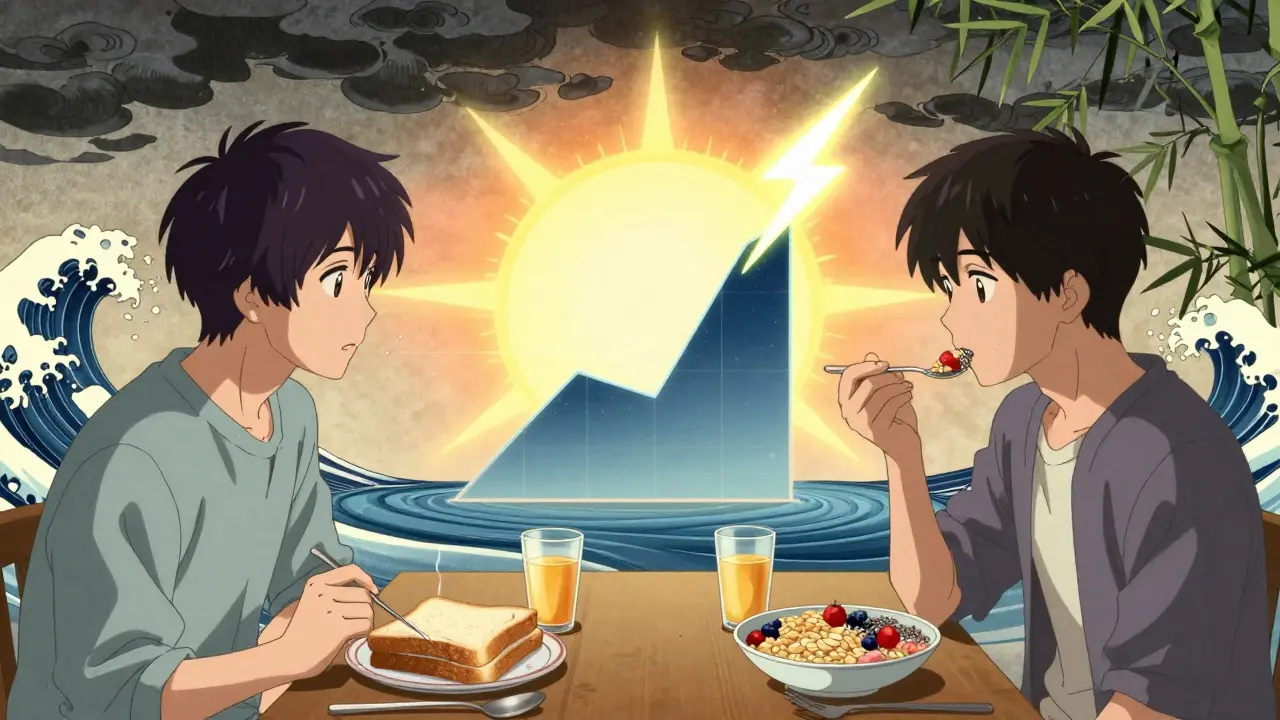
When you eat a bowl of white rice or a slice of white bread, your blood sugar spikes fast - and so does your insulin. That spike doesn’t just fade away. It leaves you hungry again within hours, often craving more carbs. This cycle isn’t just about energy. It’s tied to how your body stores fat. The low-GI diet flips this script by focusing on foods that don’t cause those sharp rises. It’s not about cutting carbs. It’s about choosing the right ones.
What Is the Glycemic Index, Really?
The glycemic index (GI) is a simple scale from 0 to 100 that tells you how quickly a food raises your blood sugar after you eat it. Pure glucose? That’s 100. White bread? Around 75. Foods with a GI of 55 or less are considered low-GI. Think lentils (GI=32), apples (GI=36), oats (GI=55), and broccoli (GI=15). High-GI foods? Think corn flakes (GI=81), baked potatoes (GI=85), and sugary cereals.
This isn’t just theory. In a 2019 study published in the American Journal of Clinical Nutrition, people on a low-GI diet saw their post-meal blood sugar spikes drop by 30-40% compared to those eating high-GI meals. That’s a big deal. When your blood sugar doesn’t crash after a meal, you’re less likely to feel shaky, tired, or hungry again too soon.
Why Low-GI Might Help With Weight Control
Here’s the common belief: low-GI foods keep you full longer. That’s because they digest slowly. Fiber, fat, and acid in foods like beans, nuts, and whole grains slow down how fast sugar enters your bloodstream. That means your body doesn’t need to pump out as much insulin. And insulin? It’s the main fat-storage hormone. Less insulin spike = less fat storage.
Dr. David Ludwig from Harvard has argued that low-GI diets may even help your body burn more calories. His research suggests people on low-GI diets could burn an extra 50-100 calories per day just by stabilizing insulin. That’s roughly the energy in a small apple - every single day. Over a year, that adds up.
But here’s the catch: when researchers control calories, the weight loss difference disappears. A 2022 analysis from the American Institute for Cancer Research looked at 12 studies with over 1,300 people. When everyone ate the same number of calories, low-GI diets didn’t lead to more weight loss than high-GI diets. So, it’s not magic. It’s not a free pass to eat more. It’s about how the food makes you feel - and how that changes your habits.
What Foods Actually Belong on a Low-GI Diet?
Not all low-GI foods are healthy. Chocolate cake has a GI of 38. Ice cream? 37. But they’re loaded with sugar and saturated fat. That’s why experts don’t recommend eating them just because they’re low-GI.
Real low-GI foods are whole, minimally processed, and rich in fiber:
- Legumes: Lentils (GI=32), chickpeas (GI=28), black beans (GI=30)
- Whole grains: Barley (GI=25), oats (GI=55), quinoa (GI=53)
- Fruits: Apples (GI=36), pears (GI=38), berries (GI=40)
- Vegetables: Broccoli (GI=15), spinach (GI=15), carrots (GI=39)
- Nuts and seeds: Almonds (GI=0), chia seeds (GI=1)
- Dairy: Plain yogurt (GI=14), milk (GI=30)
What to avoid? Refined grains, sugary snacks, white potatoes, and most breakfast cereals. Even whole wheat bread can be high-GI (GI=71) if it’s finely ground. Look for coarser textures - stone-ground, sourdough, or sprouted options tend to be lower.
How Food Prep Changes the GI
It’s not just what you eat - it’s how you cook it. Overcook pasta? GI jumps from 45 to 65. Let a banana ripen? Its GI rises from 30 to 51. Cooling cooked potatoes or rice lowers their GI because it forms resistant starch - a type of fiber your body doesn’t digest.
Adding vinegar, lemon juice, or olive oil to a meal can also lower its overall GI. A study in the Journal of Nutrition Education and Behavior found that a salad with vinaigrette had a 20% lower glycemic response than the same salad without dressing. Small changes matter.
Does the Low-GI Diet Work Better Than Other Diets?
Let’s compare it to what’s popular.
Low-carb diets (like keto) cut carbs hard. They work for weight loss - but many people struggle to stick with them long-term. A 2007 study in JAMA found that low-GI and low-carb diets led to similar weight loss after a year. But the low-GI group had better cholesterol numbers. LDL dropped 8-10% versus 5-7% in the low-carb group.
Calorie-restricted diets work - if you stick to them. But they don’t fix cravings. Low-GI diets help reduce hunger naturally. You’re not fighting your body. You’re feeding it better.
Here’s the truth: no single diet works for everyone. A 2018 DIETFITS trial, funded by the NIH with over $5 million, found no difference in weight loss between low-GI and high-GI groups after 12 months. Both lost about 6.5 kg. The winner? Consistency. People who stuck to any plan - low-GI, low-fat, or low-carb - lost weight. The diet didn’t matter as much as the habit.
Real-World Challenges
One big problem? The GI isn’t the same for everyone. A 2015 study from the Weizmann Institute in Israel showed that two people eating the same meal could have blood sugar responses that differed by 15-20 GI points. Your gut bacteria, sleep, stress, and even the time of day affect how your body reacts.
That’s why some experts - like Dr. John Sievenpiper from the University of Toronto - say the real value of low-GI foods isn’t weight loss. It’s better heart health. A 2021 review found low-GI diets lowered LDL cholesterol by 4.7 mg/dL on average. That’s a measurable drop in heart disease risk.
Another issue? Labeling. In Australia and New Zealand, you’ll see the GI Symbol on over 2,500 products. In the U.S.? Almost none. The FDA doesn’t allow GI claims on food labels. So you’re on your own. You need to learn what’s low-GI. Apps and charts help - but they’re not perfect.

How to Start a Low-GI Diet (Without Overcomplicating It)
You don’t need to memorize 3,500 GI values. Here’s how to begin:
- Swap white rice for barley or brown rice.
- Choose steel-cut oats over instant oatmeal.
- Eat whole fruit instead of juice.
- Snack on nuts or yogurt instead of crackers.
- Add beans to salads and soups.
- Let cooked potatoes and rice cool before eating.
- Use vinegar or lemon juice in dressings.
Focus on adding good foods, not just removing bad ones. The American Diabetes Association recommends 45-60 grams of carbs per meal - but they don’t tell you to count GI. They say: choose whole grains, fruits, and vegetables. That’s the low-GI diet in disguise.
Who Benefits Most?
If you have prediabetes or type 2 diabetes, the low-GI diet has strong evidence behind it. A 2019 review of 54 studies showed it lowered HbA1c (a key blood sugar marker) by 0.5% - enough to delay or prevent diabetes progression.
It’s also helpful if you’re prone to energy crashes, mid-afternoon cravings, or unexplained hunger. If you’ve tried calorie counting and still feel hungry, low-GI foods might help your body regulate itself.
But if your main goal is rapid weight loss? You’ll likely see better results from calorie control and protein-rich meals. The low-GI diet shines when you’re thinking long-term - better energy, fewer cravings, and lower risk of heart disease.
The Bottom Line
The low-GI diet isn’t a quick fix. It’s not a magic bullet. But it’s one of the few eating patterns that works with your body’s natural rhythms instead of against them. It doesn’t demand extreme restriction. It just asks you to choose whole, fiber-rich, minimally processed foods.
And that’s something everyone can agree on: better food choices lead to better health. Whether you lose weight or not, your blood sugar, your energy, and your heart will thank you.
Can I eat fruit on a low-GI diet?
Yes, most fruits are low-GI. Apples, pears, berries, oranges, and cherries have GIs between 30 and 40. Even bananas are moderate (GI=51 when ripe). The key is eating whole fruit, not juice. Juice removes fiber and spikes blood sugar fast. Stick to one serving at a time - about one medium fruit or half a cup of berries.
Is the low-GI diet good for type 2 diabetes?
Yes, and it’s strongly recommended. A 2019 review of 54 studies found that low-GI diets lowered HbA1c by 0.5% on average - enough to reduce complications. The European Association for the Study of Diabetes gives it a Grade A recommendation based on 27 clinical trials. It helps stabilize blood sugar, reduces insulin spikes, and improves long-term control.
Do I need to count GI values every day?
No. Most people don’t need to. The American Diabetes Association recommends focusing on food quality instead: choose whole grains, legumes, vegetables, and fruits. You’ll naturally eat more low-GI foods without tracking numbers. Use a GI chart for guidance when trying new foods, but don’t stress over every meal.
Are all low-GI foods healthy?
No. Chocolate cake (GI=38) and ice cream (GI=37) are low-GI but high in sugar and saturated fat. The goal isn’t to eat low-GI junk. It’s to choose nutrient-dense, fiber-rich foods that happen to be low-GI. Prioritize beans, lentils, oats, nuts, and non-starchy vegetables over processed snacks.
Why do some studies say low-GI diets don’t help with weight loss?
Because when calories are controlled, weight loss is mostly about energy balance. A 2022 analysis of 12 studies found no difference in weight loss between low-GI and high-GI diets when people ate the same number of calories. The low-GI diet’s real benefit is reducing hunger and cravings, which makes it easier to stick to a healthy eating pattern - not because it burns more fat.
