Otitis Media: When Antibiotics Are Necessary for Ear Infections

Otitis Media is the medical term for a middle ear infection. It occurs when fluid builds up behind the eardrum, often due to a cold or allergies. This trapped fluid becomes a breeding ground for bacteria or viruses, causing pain and swelling. According to the Children's Hospital of Philadelphia, over 80% of children experience at least one middle ear infection by age 3. Understanding when antibiotics for otitis media are necessary can prevent unnecessary use and reduce resistance.
What Causes Middle Ear Infections?
Most ear infections happen when the Eustachian tube - a small passage connecting the middle ear to the back of the throat - gets blocked. This tube normally drains fluid and equalizes pressure. When it’s blocked by swelling from a cold, allergies, or sinus infection, fluid builds up behind the eardrum. This creates the perfect environment for bacteria or viruses to multiply. Common bacterial culprits include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Viruses like rhinoviruses or RSV also cause infections. Risk factors include exposure to cigarette smoke (which increases infection risk by 50%), attending daycare (children there have 2-3 times more infections), and bottle-feeding while lying down. Kids under 3 are most vulnerable because their Eustachian tubes are shorter and more horizontal than adults’.
Common Symptoms to Watch For
Ear infections often start with sudden ear pain, especially at night. Other signs include fever (usually above 100.4°F), trouble sleeping, tugging at the ear, fussiness in infants, and difficulty hearing. You might notice fluid draining from the ear if the eardrum ruptures. However, ear tugging alone doesn’t always mean an infection. Doctors emphasize looking for multiple symptoms together. For example, a child with a runny nose and ear pain is more likely to have an infection than one who only tugs at their ear. If symptoms last more than 48 hours or worsen, it’s time to see a doctor. The American Academy of Pediatrics notes that 80% of uncomplicated ear infections resolve on their own within three days without antibiotics.
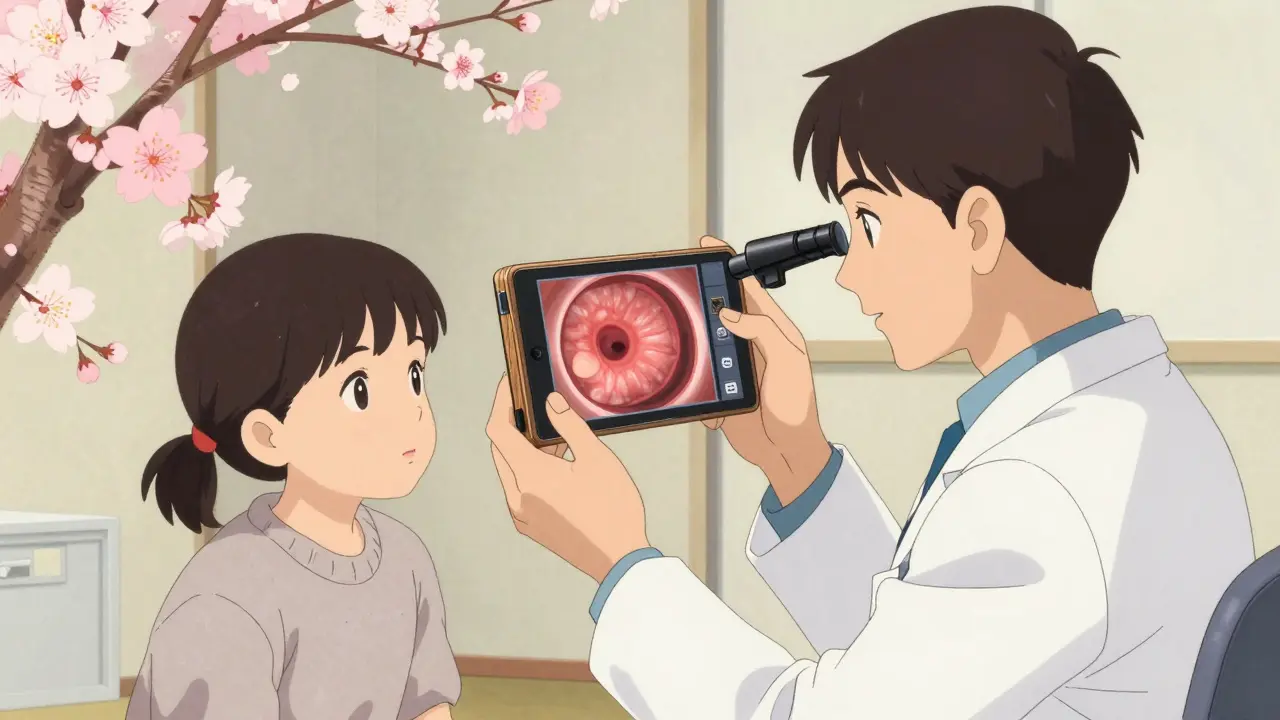
How Doctors Diagnose Ear Infections
Diagnosis starts with a physical exam using a tool called a pneumatic otoscope. This device lets the doctor look inside the ear and check eardrum movement. A healthy eardrum bounces back when air is puffed in. In an infection, the eardrum appears red, bulging, and doesn’t move well. Some clinics now use smartphone attachments like CellScope Oto to capture eardrum images for remote assessment. This has shown 85% accuracy compared to in-person exams. Audiometric tests may also be done to check for hearing loss, which typically ranges from 15 to 40 decibels during an active infection. No blood tests or X-rays are needed for routine cases. The key is confirming fluid buildup and inflammation behind the eardrum - not just redness, which can happen with other issues.

When Antibiotics Are Needed
Antibiotics aren’t always necessary. The CDC and American Academy of Pediatrics guidelines say antibiotics should be used only for specific cases. For children under 2 years with bilateral ear infections (both ears), antibiotics are recommended. For children 2-12 years with severe symptoms - like high fever (102.2°F or higher) or severe ear pain lasting over 48 hours - antibiotics are also needed. In these cases, amoxicillin is the first choice at 80-90 mg per kg per day. For penicillin-allergic kids, alternatives like ceftriaxone (a single shot) or azithromycin (a 5-day course) are used. However, for mild cases in older children, doctors often recommend waiting 48-72 hours to see if symptoms improve without antibiotics. This approach reduces unnecessary antibiotic use and helps fight resistance.
| Age | Symptoms | Antibiotic Recommendation |
|---|---|---|
| Under 2 years | Bilateral AOM or severe symptoms | Amoxicillin prescribed |
| 2-12 years | Unilateral AOM, mild symptoms | Watchful waiting for 48-72 hours |
| Any age | Severe pain or fever over 102°F | Antibiotics recommended |
Why Watchful Waiting Works
Many parents worry about waiting, but evidence shows it’s safe for most cases. A 2022 study in Pediatrics found that office-based tympanometry (a hearing test) reduced unnecessary antibiotic prescriptions by 22% in young children. When doctors recommend watchful waiting, they usually advise giving pain relief first and monitoring symptoms. For example, if a 3-year-old has mild ear pain and no fever, the doctor might say: "Try ibuprofen for 48 hours. If the pain doesn’t improve, call us." This approach avoids side effects like diarrhea (which happens in 10-25% of antibiotic users) and helps prevent antibiotic resistance. The CDC reports that 30-50% of Streptococcus pneumoniae strains are resistant to penicillin, but high-dose amoxicillin still works well for most cases. Overusing antibiotics makes resistance worse, so saving them for necessary cases is critical.
Pain Management Is Key
While waiting or even when antibiotics are used, pain control is the top priority. Acetaminophen (10-15 mg per kg per dose) or ibuprofen (5-10 mg per kg per dose) should be given every 4-6 hours. Warm compresses on the ear can also help. For severe pain, doctors may prescribe numbing ear drops like Auralgan - but only if the eardrum isn’t ruptured. Parents often report success with these strategies. One Reddit user shared: "Ibuprofen every 6 hours made the difference between constant crying and manageable discomfort." Avoid putting anything in the ear canal if there’s drainage, as this could worsen infection. Also, keep the child hydrated and upright during feeding to reduce ear pressure.
Red Flags That Need Immediate Care
Most ear infections are manageable at home, but certain symptoms require urgent attention. Call a doctor right away if you notice: fever over 104°F, severe pain unresponsive to pain relievers, pus or bloody drainage from the ear, dizziness, facial weakness, or swelling behind the ear. These could signal complications like a ruptured eardrum or mastoiditis (an infection of the skull bone). Also, if symptoms last longer than 72 hours without improvement, it’s time to revisit the doctor. Recurrent infections (three or more in six months) may need further evaluation, possibly from an ear, nose, and throat specialist.
Future Trends in Treatment
Research is advancing how we treat ear infections. The FDA-approved 15-valent pneumococcal vaccine (Vaxneuvance) shows promise in reducing vaccine-type infections. Early trials suggest it could cut pneumococcal ear infections by up to 85%. Point-of-care bacterial tests are also emerging. Dr. Peter Roland of UT Southwestern predicts these tests will guide targeted antibiotic use within five years, reducing broad-spectrum prescriptions by 30-40%. Meanwhile, probiotics and alternative treatments haven’t shown consistent benefits - a 2022 Cochrane review found no significant reduction in infection rates with probiotics. The focus remains on smarter antibiotic use and better prevention through vaccines.
Do all ear infections need antibiotics?
No. About 80% of uncomplicated ear infections resolve on their own within three days without antibiotics. Doctors typically recommend antibiotics only for children under 2 with bilateral infections, severe symptoms like high fever, or cases that don’t improve after 48-72 hours of pain management.
What’s the best pain relief for ear infections?
Acetaminophen or ibuprofen are the safest options. Give them every 4-6 hours as needed. Warm compresses on the ear can also help. Avoid putting drops in the ear if there’s drainage, as this might indicate a ruptured eardrum.
Why is watchful waiting recommended?
Watchful waiting avoids unnecessary antibiotics, which can cause side effects like diarrhea and contribute to antibiotic resistance. Studies show most mild infections clear up on their own. The CDC reports that 30-50% of common ear infection bacteria are already resistant to penicillin, making smart antibiotic use critical.
Can ear infections cause hearing loss?
Temporary hearing loss (15-40 decibels) can happen during active infection due to fluid buildup. This usually resolves once the infection clears. Persistent fluid (otitis media with effusion) may last up to three months but rarely causes permanent hearing loss. If hearing issues continue after treatment, see an ENT specialist.
How can I prevent ear infections?
Preventive steps include breastfeeding upright (reduces risk compared to bottle-feeding lying down), avoiding secondhand smoke, ensuring kids get the pneumococcal vaccine (PCV13), and washing hands frequently to reduce colds. Children in daycare have higher infection rates, but good hygiene practices can help lower risk.
