Quality Control in Manufacturing: Safety Standards That Protect Patients

When a pacemaker is implanted, an insulin pump is worn, or a surgical tool is used in an operating room, no one should have to wonder if it will work. That certainty doesn’t happen by accident. It’s the result of quality control in manufacturing - a tightly woven system of rules, checks, and processes designed to catch errors before a single device reaches a patient. In medical manufacturing, quality isn’t just about meeting specs. It’s about stopping harm before it starts.
Why Quality Control Isn’t Optional in Medical Manufacturing
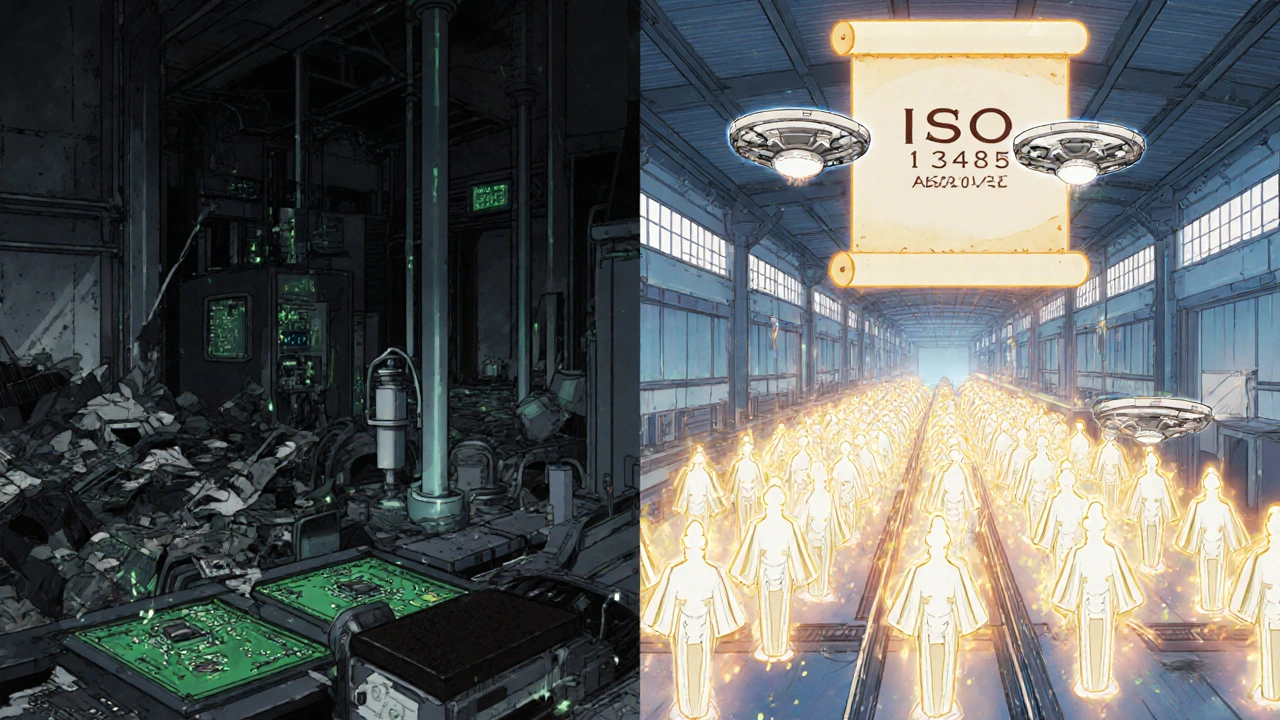
Think about what happens when a device fails. A defective glucose monitor gives wrong readings. A ventilator shuts off mid-use. A sterile syringe contains a particle that causes infection. These aren’t hypotheticals. They’ve happened. And every time, they trace back to a breakdown in quality control. The U.S. Food and Drug Administration (FDA) estimates that strong quality systems prevent about 30% of device failures that could otherwise reach patients. That’s not a small number. That’s tens of thousands of avoided injuries or deaths each year. Dr. Jeffrey Shuren, head of the FDA’s Center for Devices and Radiological Health, put it plainly: robust quality management systems prevent an estimated 200,000 adverse events annually. This isn’t about being perfect. It’s about being predictable. Every step - from the raw materials coming in to the final product leaving the factory - must be controlled. One missed inspection, one untrained worker, one unverified supplier, and the whole chain can break.The Two Big Rules: FDA 21 CFR Part 820 and ISO 13485:2016
For decades, medical device makers in the U.S. followed the FDA’s Quality System Regulation (21 CFR Part 820). This rule laid out 11 key areas manufacturers had to control: design, production, purchasing, training, documentation, and more. It worked, but it was U.S.-only. Meanwhile, companies selling in Europe, Canada, Australia, and over 30 other countries had to follow ISO 13485:2016 - an international standard focused on risk management and consistent quality across the entire lifecycle of a device. The result? Manufacturers spent extra time, money, and resources to run two parallel systems. One for the U.S. market. Another for everywhere else. That changed on January 31, 2024, when the FDA announced its Quality Management System Regulation (QMSR) Final Rule. Starting February 2, 2026, the FDA will officially adopt ISO 13485:2016 as its standard. No more dual compliance. No more redundant paperwork. This isn’t just a paperwork fix. It’s a safety upgrade. ISO 13485:2016 builds risk management into every part of the process - not as an add-on, but as the foundation. It forces companies to ask: What could go wrong? How likely is it? What are we doing to stop it?How Quality Control Actually Works in the Factory
Quality control isn’t a single step. It’s a chain of checks, each one catching what the last one might have missed.- Incoming inspection: Every component - from a tiny circuit board to a plastic housing - is tested before it’s used. Is it the right material? Is it clean? Is it from an approved supplier?
- In-process verification: During assembly, random samples are pulled and tested. Is the solder joint strong enough? Is the seal airtight? Is the software loaded correctly?
- Final product testing: Every device goes through a full functional test. For electrical devices, that means passing IEC 60601-1 safety standards: 1,500-volt dielectric strength tests, leakage current under 100 microamperes, and more.
- Statistical process control (SPC): Instead of checking every single unit, manufacturers use data to spot trends. If a machine starts producing parts that are 0.02mm too thick, SPC flags it before thousands are made.
What Happens When Quality Control Fails
The FDA’s warning letter database tells a clear story. In 2023, 41% of warning letters cited failures in supplier quality oversight. That means companies trusted vendors who didn’t meet standards. Another 23% of inspections found “paper quality systems” - documents that looked perfect on paper but didn’t reflect what was actually happening on the factory floor. Dr. Marc Jacobi, a former FDA reviewer, warned that this is the most dangerous trap. Companies think they’re compliant because they have binders full of procedures. But if no one trains staff on them, or if they’re ignored during rush hours, they’re useless. One manufacturer on Reddit shared that after implementing ISO 13485:2016, their corrective action cycle dropped from 45 days to 17. But it took 18 months of training. That’s the real cost of quality - time, effort, and culture change.The Real Cost of Cutting Corners
Some companies think quality control is an expense. It’s not. It’s an investment - and a shield. Manufacturers using ISO 13485:2016 with strong risk management saw 35% fewer field actions - recalls, safety alerts, and corrective notices. Facilities with mature systems achieved a 99.97% first-pass yield. That means almost every device passed testing on the first try. Those without it? Only 98.2%. That difference? It’s 17 times more defects. And then there’s the financial side. Before the FDA harmonized with ISO 13485, Class II and III device makers spent 25% more on compliance just to sell internationally. Now, that’s gone. The FDA estimates the new rule will save the industry $400 million a year.
What’s Next? AI, Automation, and the Future of Safety
The future of quality control isn’t just more inspections. It’s smarter ones. Early adopters are using artificial intelligence to analyze production data in real time. One study showed AI-driven systems cut defect rates by 25-40%. Instead of waiting for a failure, the system predicts it - based on vibration patterns, temperature shifts, or minor deviations in assembly speed. By 2027, Gartner predicts 60% of medical device quality systems will use AI analytics. That could reduce human error by up to 50%. But even with AI, the core hasn’t changed. The goal is still the same: make sure every device works as intended, every time, for every patient.How to Build a Solid Quality System (Without Getting Overwhelmed)
If you’re starting from scratch, here’s how to begin:- Map your process: Document every step from receiving materials to shipping the final product. Don’t skip anything.
- Identify critical points: Where could failure hurt a patient? That’s where you need the tightest controls.
- Train everyone: Quality isn’t just the job of the quality team. Every person on the line must understand their role in safety.
- Use software: Tools like Greenlight Guru help automate documentation and track compliance. Companies using integrated QMS platforms report 32% higher audit success rates.
- Start small, scale fast: Don’t try to fix everything at once. Pick one high-risk product line. Get it right. Then expand.
Final Thought: It’s Not About Paperwork. It’s About People.
Every procedure, every checklist, every audit - it’s all in service of one thing: protecting someone’s life. A patient doesn’t care if your system is ISO certified or FDA compliant. They care that their device works. That their IV pump doesn’t stop. That their monitor doesn’t lie. That’s what quality control is for. Not to pass an inspection. Not to check a box. But to make sure when someone needs help, the machine is ready.What is ISO 13485:2016 and why does it matter for patient safety?
ISO 13485:2016 is the international standard for quality management systems in medical device manufacturing. It requires companies to embed risk management into every process - from design to delivery. This means identifying potential failures before they happen and putting controls in place to stop them. Unlike older systems that focused only on documentation, ISO 13485:2016 demands real, observable control over production. That’s why it directly reduces patient harm: fewer defects, fewer recalls, and more reliable devices.
How does the FDA’s new QMSR rule change things for manufacturers?
The FDA’s QMSR Final Rule, effective February 2, 2026, replaces the old 21 CFR Part 820 with ISO 13485:2016. This means U.S. manufacturers no longer need to maintain two separate quality systems - one for the U.S. and another for global markets. It simplifies compliance, cuts redundant paperwork by about 30%, and aligns U.S. standards with the rest of the world. For companies selling internationally, this saves time and money. For patients, it means more consistent safety standards across all devices, no matter where they’re made.
What are the biggest mistakes manufacturers make in quality control?
The top mistakes are: relying on paperwork without real process understanding, skipping supplier audits, and not training staff properly. The FDA found that 23% of inspection findings involved complete documentation that didn’t match what happened on the floor. Another 41% of warning letters in 2023 cited poor supplier oversight. Quality isn’t about having a thick manual - it’s about making sure every person on the line knows why each step matters and how to do it right every time.
Can small manufacturers afford to implement ISO 13485:2016?
Yes - but it takes planning. While large companies have teams dedicated to compliance, smaller firms can start with a focused approach: pick one high-risk product, build a lean system around it, and use affordable tools like Greenlight Guru or open-source templates from the FDA. The FDA offers free guidance documents, and ISO 13485 implementation guides cost around $338. The real cost isn’t the tools - it’s the time spent training staff. But the payoff - fewer recalls, faster approvals, and safer devices - makes it worth it.
How does AI improve quality control in medical manufacturing?
AI analyzes real-time production data - like machine vibrations, temperature changes, or assembly times - to spot patterns that humans miss. Early adopters report 25-40% fewer defects because AI predicts failures before they happen. For example, if a laser welder starts drifting slightly off-spec, AI flags it before a batch is ruined. By 2027, Gartner predicts 60% of medical device companies will use AI-driven quality systems, reducing human error by up to half. It doesn’t replace people - it gives them better tools to protect patients.

Douglas cardoza
November 25, 2025 AT 04:37Man, I’ve seen factories where the QA team is basically ignored until something goes wrong. Then it’s all hands on deck and everyone’s scrambling. ISO 13485 finally makes it part of the culture, not just another box to check. Real change starts when the line worker knows their job is saving lives, not just hitting targets.
Also, glad they’re ditching the dual-system mess. Too many small shops were getting crushed by paperwork.
One guy I know at a med device shop said their audit pass rate jumped from 62% to 94% in 18 months after they started doing daily 10-minute huddles to review one process each day. Simple, but it stuck.
Adam Hainsfurther
November 25, 2025 AT 06:01The shift from 21 CFR Part 820 to ISO 13485:2016 isn’t just regulatory alignment - it’s a philosophical upgrade. The old system was reactive: ‘Did we document it?’ The new one is proactive: ‘Could this fail, and if so, why didn’t we stop it?’ That’s the difference between compliance and true safety culture.
It’s not about the number of forms filled out. It’s about whether the person holding the soldering iron understands why the temperature matters. That’s the real metric.
Rachael Gallagher
November 26, 2025 AT 20:26They say this is about safety but let’s be real - it’s about big pharma locking out small players. You think a startup can afford AI-driven SPC systems? Nah. They’ll just get buried under compliance costs and vanish. Then the market’s owned by five corporations who’ve been playing this game for decades.
Call it ‘patient safety’ all you want. It’s monopoly engineering disguised as regulation.
steven patiño palacio
November 27, 2025 AT 07:32It’s worth noting that ISO 13485:2016 isn’t just a checklist - it’s a framework for organizational maturity. Companies that implement it well don’t just reduce defects; they improve morale. Workers feel empowered because their input is tied to real outcomes.
One manufacturer I consulted with saw a 40% drop in near-miss reports after they started rewarding frontline staff for identifying process gaps. That’s not luck. That’s culture.
And yes, AI helps. But only if the people using it understand the context. Technology without training is just noise.
stephanie Hill
November 28, 2025 AT 01:50Did you know the FDA’s own audit reports show that 70% of ‘compliant’ facilities still had unverified suppliers? They’re all just faking it with fancy binders. And now they’re making us pay for it? This whole thing feels like a corporate tax.
Also, why does no one ever ask who’s auditing the auditors? Just saying.
And AI? Please. They’re just replacing human error with algorithmic bias. Wait till the machine misses a defect because it was trained on data from a plant in China that uses different standards. Then we’ll see who’s really safe.
Andy Louis-Charles
November 29, 2025 AT 09:13Just saw a demo of an AI system that uses thermal imaging to detect micro-cracks in catheter housings during assembly. It’s not magic - it’s math. But it caught a flaw that humans missed for 11 months. That’s one device that won’t fail inside someone’s artery.
And yeah, the cost of implementation is real. But the cost of a recall? Millions. And a life? Priceless.
Tools like Greenlight Guru are game-changers for small teams. No need to hire a full-time compliance officer. Just plug in your process and let the software flag the gaps.
Akash Chopda
December 1, 2025 AT 08:58They say ISO 13485 saves lives but what about the workers in factories who get sick from chemicals because the suppliers arent checked properly? Nobody talks about that. The FDA cares about devices not the people making them. This is just another way to control the poor.
And AI? They are watching everything. Soon your toaster will report you for using it wrong.
Trust the system? I dont trust anyone
Sam Jepsen
December 2, 2025 AT 04:22I’ve worked on both sides - big med device corp and a small startup. The biggest myth is that ISO 13485 is too heavy for small teams. Nah. You just need to focus on your highest-risk product. Pick one. Do it right. Then expand.
My team used free FDA templates and did weekly 15-minute ‘safety huddles’. We didn’t need fancy software. We needed consistency. And now? Our first-pass yield went from 92% to 99.1%.
It’s not about being perfect. It’s about being predictable. That’s what saves lives.
Yvonne Franklin
December 2, 2025 AT 19:46Traceability saved us last year. One batch of insulin pump batteries had a tiny voltage drift. Because we tracked every component back to the supplier and lot number, we recalled 47 units - not 12,000.
That’s the power of good systems. Not flashy AI. Not expensive consultants. Just clear records and people who actually read them.
Also, training isn’t a one-time thing. It’s a habit. Do it weekly. Make it part of the shift change.
Bartholemy Tuite
December 3, 2025 AT 03:08Look I’ve been in this game since the 90s and let me tell ya the real game changer ain’t the ISO standard or the AI or even the FDA’s new rule - it’s the fact that more people are finally starting to talk about quality like it’s not just some department that sits in the back room with a binder and a coffee machine.
My mate in Cork said they started putting QR codes on every tool that linked to the training video for that specific step. Workers could scan it on their phones during breaks. Turns out people actually watch them if they’re under 90 seconds.
And yeah the paperwork got lighter but the responsibility got heavier - and that’s a good thing. Because when you know your work could kill someone if you slip up, you don’t slack off. You don’t cut corners. You just do the damn thing right.
Also the guy who said AI is surveillance? He’s not wrong but he’s missing the point - AI doesn’t replace us, it just makes us better at being human. We still have to care.
And if you’re a small shop? Start with one product. One process. One person who gives a damn. That’s all it takes.
Neoma Geoghegan
December 4, 2025 AT 19:29ISO 13485:2016 isn’t compliance - it’s risk mitigation engineered into DNA. No more reactive firefighting. Just proactive control loops. The ROI? 35% fewer field actions. That’s not a number - that’s people going home safe.
And the timeline? 2026 is tight but doable. Start with your top 3 high-risk products. Map the critical control points. Train the floor. Automate the documentation. Done.
Stop thinking in binders. Start thinking in outcomes.