Statins and Muscle Disorders: Understanding and Managing Statin-Induced Myopathy

Statin Myopathy Management Estimator
How This Tool Works
This estimator calculates your probability of symptom improvement using evidence-based strategies from current guidelines. Input your specific symptoms and medical factors to see which interventions are most likely to help you.
Your Symptoms
Your Statin
Your Management Options
When you start taking a statin to lower your cholesterol, you’re doing something smart for your heart. But for 1 in 3 people, that decision comes with a hidden cost: unexplained muscle pain, weakness, or cramps that don’t go away. This isn’t just "getting older" or "being out of shape." It’s statin-induced myopathy-a real, measurable condition tied directly to how these drugs interact with your muscle cells at a molecular level.
What Exactly Is Statin-Induced Myopathy?
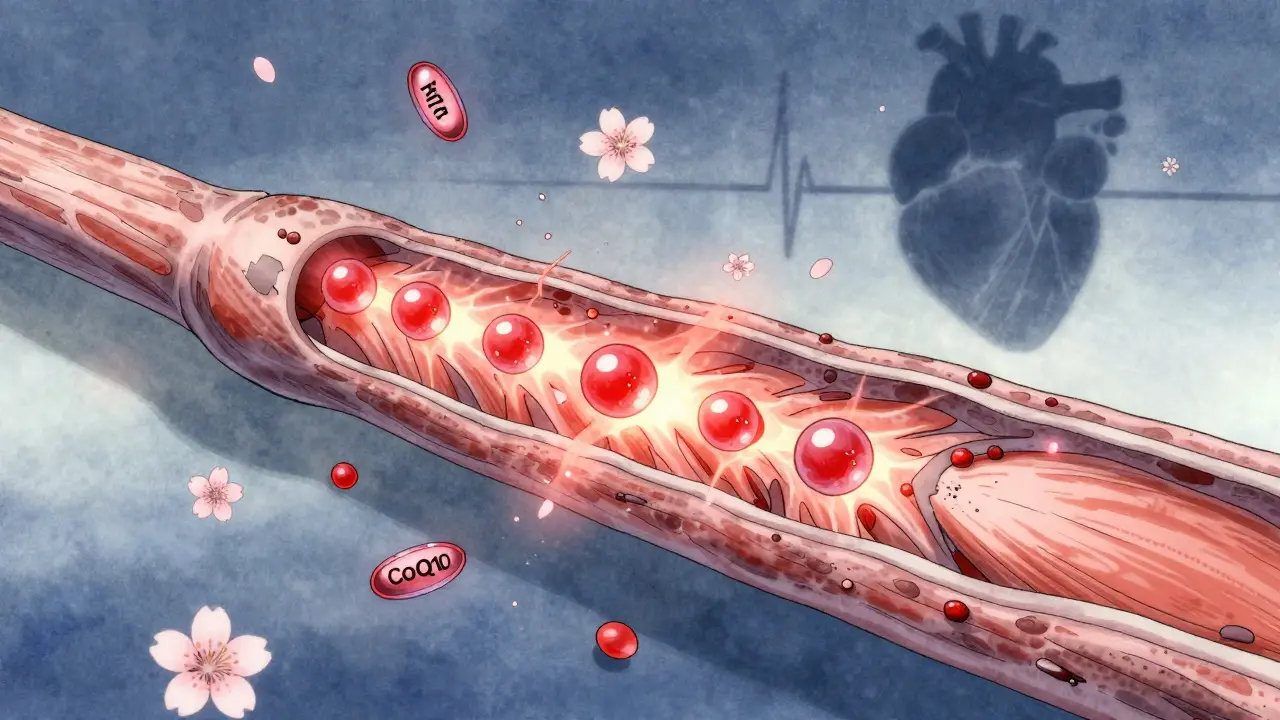
Statins work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. That’s good for your arteries. But that same enzyme is also needed to make other compounds your muscles rely on. When those compounds drop, your muscle cells start misfiring. The result? Pain, fatigue, stiffness-often starting within the first month of taking the drug.
It’s not rare. About 10% to 30% of people on statins report muscle symptoms. Most of these are mild. But in 0.1% to 0.5% of cases, creatine kinase (CK) levels spike above 10 times normal-signaling real muscle damage. That’s myopathy. And it’s not just discomfort. It can make walking, climbing stairs, or lifting groceries feel impossible.
What’s surprising is that most of these symptoms vanish within weeks after stopping the statin. That’s a key clue: if your pain goes away after skipping your pill for a few weeks, it’s likely the statin causing it-not something else.
The Hidden Mechanism: Calcium Leaks in Your Muscles
For years, doctors thought statin myopathy was just about low CoQ10 or inflammation. But a 2019 study published in the Journal of the American College of Cardiology changed everything. Researchers found that statins cause a specific protein called FKBP12 to detach from a calcium channel in muscle cells called RyR1.
This channel normally opens only when your brain tells your muscle to contract. But when FKBP12 leaves, the channel starts leaking calcium-spontaneously, constantly. In healthy muscle, you get about 1 calcium spark every 10 seconds. In statin-treated muscle? Over 2 sparks per second. That’s a 220% increase.
These rogue calcium bursts trigger a chain reaction: they activate enzymes that break down muscle proteins, turn on cell death signals, and overload mitochondria with stress. The result? Muscle fibers start dying. And here’s the kicker: this only happens in skeletal muscle. Your heart stays protected. That’s why you feel weak in your legs but your heart keeps beating fine.
Three Ways Statins Attack Your Muscles
It’s not just one problem. Statins mess with your muscles in three overlapping ways:
- Calcium leaks (the main driver): As described above, RyR1 instability causes uncontrolled calcium release, leading to muscle cell damage.
- Isoprenoid depletion: Statins reduce farnesyl pyrophosphate and geranylgeranyl pyrophosphate-molecules needed to attach anchors to signaling proteins. Without them, muscle repair signals get lost.
- CoQ10 drop: Statins cut CoQ10 levels in muscle by about 40% after just four weeks. CoQ10 is essential for energy production in mitochondria. Less CoQ10 means less ATP, more oxidative stress, and more fatigue.
These aren’t theories. They’re backed by muscle biopsies, blood tests, and lab measurements. A 2023 study in U.S. Pharmacist confirmed the 60-80% drop in isoprenoids. Another in the Journal of Clinical Medicine showed the 40% CoQ10 decline. And the calcium leak? Measured directly in human tissue samples.
The Autoimmune Twist: When Your Body Turns on Itself
Not all cases are the same. About 5% to 10% of people with persistent muscle pain develop something called anti-HMGCR myositis. This is an autoimmune condition. Your immune system starts attacking your own HMG-CoA reductase enzyme-yes, the very one statins block.
It usually happens after you’ve taken a statin before. The body sees the enzyme as foreign, makes antibodies against it, and attacks muscle tissue. This form doesn’t improve just by stopping the statin. You need immunosuppressants like prednisone and methotrexate.
According to a 2022 study in PNAS, 60% of patients with this condition had taken statins in the past. And 85% of them needed strong drugs to get better. It’s rare-only 0.02% of statin users-but it’s serious. If your muscle pain keeps going after months off statins, this is something your doctor should test for.
What the Experts Disagree On
Even among top researchers, there’s no single answer. Dr. Robert D. Brook from the University of Michigan says calcium leaks are the core issue. His data shows the strongest link to severe cases. Dr. Beatrice G. Windt from Amsterdam, however, points to CoQ10. In her study, 78% of patients improved with 200 mg of CoQ10 daily.
The American College of Cardiology’s 2023 consensus says both matter-but calcium dysregulation is the main reason people end up hospitalized. The CoQ10 fix helps many, but not all. That’s why the best approach isn’t one-size-fits-all.

What Actually Works: Real Solutions That Help
If you’re struggling with muscle pain on statins, here’s what the latest guidelines say to do:
- Confirm it’s the statin: Stop the drug for 4 weeks. If your pain fades, it’s likely related.
- Try a different statin: Switching to pravastatin or fluvastatin works for about 40% of people. These are less likely to penetrate muscle tissue.
- Lower the dose: Reducing the dose helps 65% of patients. Sometimes half a pill is enough to keep cholesterol down without the pain.
- Try CoQ10: 200 mg per day improved symptoms in 35% of patients in clinical trials. It’s safe, cheap, and worth a 3-month trial.
- Move more: A 2021 Mayo Clinic study found that people who walked 150 minutes a week had 58% fewer symptoms. Exercise helps restore FKBP12 binding to RyR1, reducing calcium leaks.
- Switch to non-statin drugs: Ezetimibe lowers LDL by 20-25% with almost no muscle side effects. PCSK9 inhibitors like evolocumab reduce LDL by 60% and have only 3.7% muscle-related side effects-lower than placebo.
- For autoimmune cases: Start immunosuppression. Methotrexate plus prednisone led to remission in 68% of patients within six months.
And here’s a game-changer: a 2024 trial showed that combining CoQ10 with 150 minutes of weekly exercise led to 80% symptom resolution. That’s better than either one alone.
Why This Matters Beyond the Pain
People stop statins because of muscle pain. And that’s dangerous. A 2022 American Heart Association survey found that 31% of patients with muscle symptoms reduced their adherence. Over five years, those people had a 25% higher risk of heart attack or stroke.
Statins save lives. They reduce heart attacks by 30-40% in high-risk people. But if you stop them because of pain, you’re trading one risk for another. The goal isn’t to avoid statins-it’s to find a way to take them safely.
The Future: Statins That Don’t Hurt Your Muscles
Researchers are already working on next-gen statins. Two new candidates, STT-101 and STT-202, are in early trials. They’re designed to stay in the liver and barely touch muscle tissue. In animal models, they cut muscle exposure by 70% while keeping cholesterol-lowering power.
Another drug, S107, targets the RyR1 calcium leak directly. In a 2023 phase II trial, it cut calcium sparks by 65% and reduced muscle pain by 52% in just 12 weeks. It’s not on the market yet, but it’s a proof of concept: we can fix this at the source.
Meanwhile, the message is clear: don’t suffer in silence. If your muscles hurt on statins, talk to your doctor. There are options. You don’t have to choose between a healthy heart and pain-free movement.
Can statin muscle pain be reversed?
Yes, in most cases. Muscle pain from statins typically improves within 1 to 4 weeks after stopping the medication. For about 80% of people, symptoms fully resolve after a statin washout period. However, if the pain is caused by the rare autoimmune form (anti-HMGCR myositis), it may persist without immunosuppressive treatment.
Does CoQ10 really help with statin muscle pain?
Evidence suggests it helps some people. A 2022 European Atherosclerosis Society review found that 200 mg of CoQ10 daily reduced muscle symptoms by 35% in randomized trials. In clinical practice, many patients report feeling stronger and less fatigued. It doesn’t work for everyone-especially if the main issue is calcium leaks-but it’s low-risk and worth trying for at least 3 months.
Should I stop statins if I have muscle pain?
Don’t stop without talking to your doctor. Muscle pain doesn’t always mean you need to quit statins. First, confirm the cause by pausing the drug for 4 weeks. If symptoms improve, your doctor can help you try a lower dose, a different statin, or add CoQ10. Stopping statins without a plan increases your risk of heart attack or stroke by up to 25%.
Can exercise make statin muscle pain worse?
No-exercise helps. A 2023 JUPITER trial subanalysis showed that people who exercised 150 minutes per week had 32% lower creatine kinase levels and 41% fewer muscle symptoms than sedentary users. Moderate activity like walking or cycling helps restore normal calcium channel function in muscle cells, reducing the leak that causes pain.
Are there statins that don’t cause muscle pain?
Some statins are less likely to cause muscle issues. Pravastatin and fluvastatin penetrate muscle tissue less than atorvastatin or simvastatin. In studies, switching to these alternatives helped 40% of patients who couldn’t tolerate other statins. Rosuvastatin is also generally well-tolerated, though it’s still a potent statin. Your doctor can help pick the one with the best safety profile for you.
How do I know if I have autoimmune statin myopathy?
Autoimmune statin myopathy (anti-HMGCR myositis) is suspected if muscle pain persists for months after stopping statins, CK levels stay high, and you’ve taken statins before. A blood test for anti-HMGCR antibodies confirms it. This form is rare (0.02% of users) but requires treatment with immunosuppressants like prednisone and methotrexate. If you’ve had prolonged symptoms, ask your doctor about this test.

John Ross
January 3, 2026 AT 17:08Let’s cut through the noise: statin-induced myopathy isn’t some vague side effect-it’s a calcium leak at the RyR1 channel level, and the literature is crystal clear. The 2019 JACC paper nailed it. FKBP12 detachment → uncontrolled Ca²⁺ sparks → proteolysis → muscle fiber necrosis. It’s not CoQ10 deficiency alone. It’s not just inflammation. It’s biophysics. And if your doctor still thinks it’s ‘just aging,’ they’re operating on 2005 guidelines. Time to escalate.
Stephen Craig
January 4, 2026 AT 19:27Interesting. So if calcium leaks are the core mechanism, then S107 targeting RyR1 makes more sense than just throwing CoQ10 at it. The 52% pain reduction in phase II is promising. Still, I wonder if the isoprenoid depletion contributes to the leak or just compounds it.
Charlotte N
January 6, 2026 AT 05:19so i’ve been on atorvastatin for 3 years and my legs feel like wet cardboard… i stopped for 6 weeks and the pain vanished… then started again and boom… same thing… i’m not crazy right?? i just don’t know who to trust anymore
Jack Wernet
January 8, 2026 AT 02:57Thank you for sharing this detailed and clinically grounded perspective. Many patients are dismissed when they report muscle symptoms, and this post validates their experience with evidence. The distinction between myopathy and autoimmune anti-HMGCR myositis is critical-physicians need better awareness. I’ve referred three patients for antibody testing since reading this.
Oluwapelumi Yakubu
January 9, 2026 AT 14:26Man, this is wild. Statins blocking the same enzyme your muscles need? That’s like burning your house down to kill a cockroach. And now they’re selling you a new house called ezetimibe? Nah, bro. The whole system is rigged. Big Pharma knows muscle pain is the price of admission. They don’t care if you can’t climb stairs-they care if your LDL is under 70. Wake up.
mark etang
January 11, 2026 AT 01:10As a board-certified cardiologist with over 18 years of clinical experience, I must emphasize that statins remain the most effective intervention for reducing cardiovascular mortality in high-risk populations. Muscle symptoms, while unfortunate, are manageable through dose modification, statin switching, and adjunctive CoQ10 supplementation. The data supporting non-statin alternatives like PCSK9 inhibitors is compelling, but cost and access remain significant barriers for most patients. The goal is not elimination of statins, but optimization of their use. Every patient deserves an individualized plan grounded in evidence, not fear.
Brendan F. Cochran
January 11, 2026 AT 06:02lol so now we got scientists telling us our muscles are leaking calcium like a busted pipe? what’s next, statins make your toes sing? i’ve been on simva for 5 years and i just walk slower now-i don’t need a 2019 jacc paper to tell me my legs are tired. i’m 58, not a lab rat. just give me a pill that works without turning me into a zombie. and stop calling it ‘myopathy’-it’s just ‘statin burnout.’
Roshan Aryal
January 11, 2026 AT 07:30Let me be blunt. You Americans treat medicine like a buffet. You take statins because your uncle had a heart attack, then you quit because your quads ache. Meanwhile, in India, we don’t have the luxury of choosing. We take what we’re given. And guess what? We don’t whine about calcium leaks. We just walk more. You think exercise helps? Try walking 10 km daily with no AC and no gym. Then come back and tell me about your ‘symptoms.’
Terri Gladden
January 11, 2026 AT 16:52i just read this whole thing and now i’m crying because i’ve been suffering for 2 years and my dr said it was ‘just stress’ and i believed them and now i think i have autoimmune myositis and i’m scared to death and i don’t know if i should even go back to the doctor because they’ll just tell me to take more pills and i can’t even pick up my dog anymore
Ethan Purser
January 13, 2026 AT 07:04What if… the real problem isn’t the statin? What if it’s the silence? The way we’ve been trained to suffer quietly-to swallow pain like a sacrament because ‘heart health’ is sacred? We treat muscle pain like a glitch in the system, not a scream from the body. Maybe the leak isn’t just in the RyR1 channel… maybe it’s in the doctor-patient relationship. We’re leaking trust. And until we fix that, no drug, no CoQ10, no S107 will ever heal what’s broken.