Antiplatelet Drugs – A Quick Guide
Ever wonder why your doctor puts you on a pill called “antiplatelet”? In simple terms, these meds stop tiny blood cells called platelets from sticking together and forming clots. When clots block a heart artery or a brain vessel, you can end up with a heart attack or stroke. So, antiplatelet drugs act like a traffic cop, keeping the flow smooth and the dangers low.
How Antiplatelet Drugs Work
Platelets are like the body’s emergency patches. They rush to any cut and clump together to stop bleeding. In some people, especially those with heart disease, the clotting system gets a bit over‑zealous. Antiplatelet drugs interfere with the chemical signals that tell platelets to stick. The most common signal blocker is aspirin, which disables an enzyme called COX‑1. Other drugs, such as clopidogrel, block a different receptor (P2Y12), giving doctors more options if aspirin alone isn’t enough.
Common Antiplatelet Medications
Aspirin – The oldest and cheapest. One low‑dose tablet a day can reduce the risk of a second heart attack. It’s easy to take but can irritate the stomach, so many doctors suggest taking it with food or a coated version.
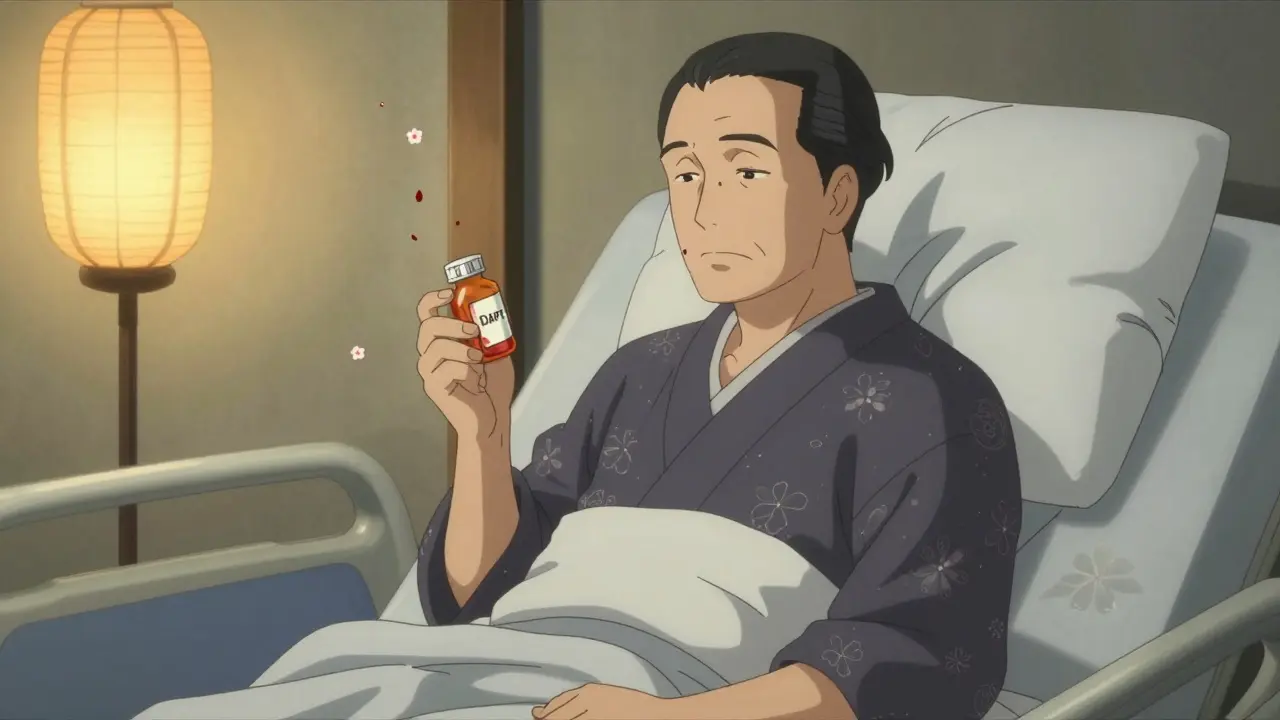
Clopidogrel (Plavix) – Often prescribed after a stent is placed or if a patient can’t tolerate aspirin. It works on a separate pathway, so it’s a good backup or combo partner.
Ticagrelor (Brilinta) and Prasugrel (Effient) – Newer agents that act faster than clopidogrel. They’re usually reserved for acute coronary syndrome or after certain surgeries.
Dipyridamole – Not as common on its own, but sometimes paired with aspirin for stroke prevention.
Even though these drugs share a goal—prevent clots—they have different side‑effect profiles. Bleeding is the big one to watch for. If you notice unusual bruises, nosebleeds, or blood in the stool, call your doctor right away.
Here are a few practical tips to keep your antiplatelet therapy safe:
- Take the medication exactly as prescribed. Missing doses can let platelets revert to their sticky state.
- Tell every health‑care provider you see that you’re on an antiplatelet drug, especially before any surgery or dental work.
- Avoid over‑the‑counter NSAIDs (like ibuprofen) unless your doctor says it’s okay—they can increase bleeding risk.
- Watch your diet. Foods high in vitamin K (like kale) don’t affect antiplatelet drugs, but alcohol can amplify bleeding.
- Keep a list of all your meds. Some prescriptions, like certain blood thinners, can interact badly with antiplatelets.
Most people stay on antiplatelet drugs for years, sometimes for life. That long‑term use is why regular check‑ups matter. Your doctor may order blood tests to make sure you’re not getting too much bleed or too little clot prevention.
Bottom line: antiplatelet drugs are a cornerstone of heart‑ and brain‑health protection. They’re not magic pills, but when used correctly, they dramatically cut the odds of a serious clot. Talk to your pharmacist if you’re unsure about any side effect, and never stop a dose without a professional’s go‑ahead.
Got more questions about a specific drug or how it fits into your treatment plan? Drop a comment below or reach out to your health‑care team. Staying informed is the best way to keep your blood flowing the right way.
Learn how to manage bleeding risks from dual antiplatelet therapy after a heart stent or heart attack. Discover safer alternatives, when to shorten treatment, and how to live well without fear of bleeding.
- Read More

Thinking about switching from Clopidogrel? Here’s your straight-up guide to seven real-world alternatives, breaking down how they work, their upsides, and what you’ll want to watch out for. Not all blood thinners are created equal—each alternative comes with its own twist, fitting into specific situations. Find out what makes each one tick, what to expect if you’re prescribed one, and when they tend to work best. You’ll also get a no-nonsense table comparing them side by side for easy decisions. If you need to talk options with your doctor, you’ll have all the basics covered.
