Types of Hearing Loss: A Complete Guide

Hearing Loss Type Calculator
Identify Your Hearing Loss Type
Answer the following questions to help identify which type of hearing loss may be affecting you.
When we talk about Hearing loss is a permanent or temporary reduction in the ability to perceive sounds, most people picture a single problem. In reality, there are several distinct categories, each with its own causes, symptoms, and treatment paths. This guide pulls apart the main types of hearing loss so you can recognize what’s happening and take the right next steps.
Key Takeaways
- Hearing loss falls into three primary groups: conductive, sensorineural, and mixed.
- Age‑related (presbycusis) and noise‑induced loss are the most common sensorineural forms.
- Accurate diagnosis uses audiometry, tympanometry, and sometimes imaging.
- Treatment ranges from simple ear‑wax removal to hearing aids, cochlear implants, or surgery.
- Early detection and proper management dramatically improve quality of life.
What Is Hearing Loss?
Hearing loss describes any reduction in the ability to detect, differentiate, or understand sounds. It can affect one ear or both, and may develop suddenly or over years. The condition is measured in decibels (dB) using an audiogram, which plots the softest sounds a person can hear across different frequencies.
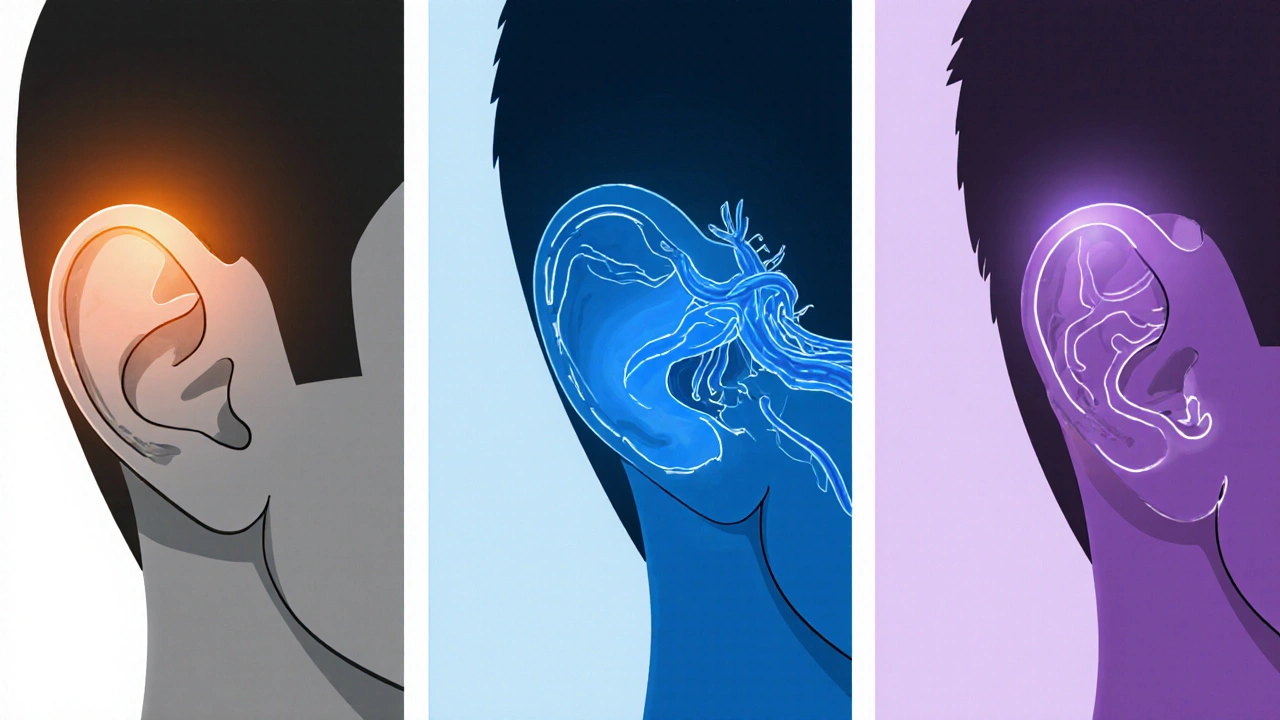
Main Types of Hearing Loss
Understanding which type you have guides treatment. Below are the most frequently encountered categories.
Conductive hearing loss is a problem that blocks sound from traveling through the outer or middle ear to the inner ear
Common causes include ear‑wax buildup, fluid from middle‑ear infections (otitis media), a perforated eardrum, or abnormal bone growth (otosclerosis). Conductive loss usually improves when the blockage is cleared or the underlying condition is treated.
Sensorineural hearing loss is a damage to the inner ear hair cells or the auditory nerve pathways
This is the most prevalent form in adults. It can be caused by aging (presbycusis), prolonged exposure to loud noise, genetic mutations, certain medications (ototoxic drugs), or illnesses such as Meniere’s disease. Damage is often permanent, so amplification or implantation is usually needed.
Mixed hearing loss is a combination of conductive and sensorineural components
Patients with chronic ear infections that also have age‑related inner‑ear decline often fall into this category. Managing mixed loss typically involves addressing the conductive part first, then providing amplification for the sensorineural component.
Auditory neuropathy spectrum disorder is a condition where the inner ear receives sound, but the auditory nerve fails to transmit it correctly
Individuals may hear sounds but struggle to understand speech, especially in noisy settings. Early diagnosis is crucial because hearing aids help only some patients; cochlear implants are often more effective.
Presbycusis is a gradual, age‑related decline in hearing sensitivity, primarily affecting high frequencies
By age 65, about one‑third of people show signs of presbycusis. Genetics, cumulative noise exposure, and vascular changes all play a role. The loss is sensorineural, making hearing aids the standard solution.
Noise‑induced hearing loss is a damage caused by exposure to loud sounds, either a single intense event or repeated exposure over time
Construction workers, musicians, and frequent concert‑goers are at risk. The damage often appears first at 4‑6 kHz on an audiogram and can be permanent if protective measures aren’t used.
Quick Comparison of the Most Common Types
| Type | Part Affected | Typical Cause | Common Symptoms | Primary Treatment |
|---|---|---|---|---|
| Conductive | Outer/Middle ear | Ear‑wax, otitis media, perforated eardrum | Muffled sound, hearing improves with ear cleaning | Medical/surgical correction, hearing aid if needed |
| Sensorineural | Inner ear or auditory nerve | Presbycusis, loud noise, ototoxic drugs | Difficulty hearing high pitches, speech in noise | Hearing aids, cochlear implant for severe cases |
| Mixed | Both conductive & sensorineural | Chronic infections + age‑related loss | Combination of muffled and unclear speech | Treat conductive part, then amplification |
| Auditory neuropathy | Auditory nerve pathways | Neural dys-synchrony, often genetic | Sounds heard but speech is garbled | Cochlear implant (most effective) |
How Professionals Diagnose Different Types
Accurate diagnosis starts with a thorough case history-when did you notice the loss? Any recent illness, medication, or noise exposure? From there, audiologists run a series of tests.
Audiometry is a standard hearing test that measures the softest sounds a person can detect across frequencies
The results plot on an audiogram. Conductive loss shows a gap between air‑ and bone‑conduction thresholds, while sensorineural loss shifts both equally.
Tympanometry
This test evaluates middle‑ear pressure and eardrum mobility, pinpointing conductive problems like fluid or ossicular chain issues.
Otoacoustic Emissions (OAEs)
OAEs assess outer‑hair‑cell function. A normal OAE with abnormal audiometry suggests a neural issue such as auditory neuropathy.
Auditory Brainstem Response (ABR)
ABR measures neural timing from the ear to the brainstem, helping differentiate between cochlear and neural pathologies.
Treatment Options Tailored to Each Type
Once the type is clear, options can be matched.
Conductive Loss
- Ear‑wax removal or ear‑tube placement for fluid.
- Osseointegrated devices (Bone‑anchored hearing aids) if surgery is needed.
Sensorineural Loss
- Digital hearing aids-customized amplification, noise reduction, directional microphones.
- Cochlear implants for moderate‑to‑severe cases where hearing aids no longer help.
- Assistive listening devices (phone amplifiers, TV streamers).
Mixed Loss
- Address conductive component first (e.g., tympanostomy tubes).
- Follow with hearing aids or implants for the sensorineural part.
Auditory Neuropathy
- Trials with hearing aids may help a minority.
- Cochlear implantation is often the most reliable solution.
Age‑Related (Presbycusis) & Noise‑Induced Loss
- High‑frequency hearing aids with feedback cancellation.
- Regular monitoring to adjust settings as loss progresses.
- Preventive measures: earplugs, volume limits on devices.
Living Well With Hearing Loss
Technology is only part of the picture. Everyday habits can make a huge difference.
- Face the speaker - visual cues boost comprehension.
- Ask people to repeat or rephrase instead of just speaking louder.
- Use captioning on TVs, smartphones, and video calls.
- Consider a personal FM system in noisy classrooms or meetings.
- Schedule annual hearing check‑ups-early tweaks prevent frustration.

When to Seek Professional Help
If you notice any of the following, book an appointment with an audiologist or ENT specialist:
- Sudden loss in one ear.
- Persistent ringing (tinnitus) that interferes with sleep.
- Difficulty following conversations, especially on the phone.
- History of head injury or exposure to loud blasts.
Frequently Asked Questions
Can hearing loss be reversed?
Only conductive loss caused by blockage or fluid can often be fully reversed with medical treatment. Sensorineural damage is usually permanent, so management relies on amplification or implants.
How often should I get a hearing test?
Adults without risk factors should test every three years. If you work in noisy environments, have a family history, or notice changes, schedule a test annually.
Are there any over‑the‑counter solutions for mild hearing loss?
OTC hearing aids are now legal in the U.S. and many other countries for mild‑to‑moderate loss. They can be a cost‑effective first step, but a professional fitting often yields better outcomes.
What’s the difference between a hearing aid and a cochlear implant?
A hearing aid amplifies sound and relies on a functional cochlea. A cochlear implant bypasses damaged hair cells, converting sound into electrical signals that directly stimulate the auditory nerve.
Can children develop the same types of hearing loss as adults?
Yes, children can experience conductive loss from chronic ear infections or congenital malformations, and genetic sensorineural loss that may be present at birth or develop later.
Next Steps
Start by scheduling a basic audiometry screening. Bring a list of any recent noises, medications, or ear problems you’ve had. If a specific type is identified, follow the tailored treatment plan-whether it’s a simple cleaning, a hearing aid fitting, or a referral for a cochlear‑implant evaluation.
Remember, hearing loss isn’t a life sentence. With the right diagnosis and tools, you can stay connected to conversations, music, and the world around you.

Christopher Eyer
October 15, 2025 AT 18:28While the article attempts to be comprehnsive, it glosses over the nuanced interplay between genetics and environmental factors. A more critical analysis would have highlighted recent epigenetic research, which this piece entirely omits.
Welcher Saltsman
October 17, 2025 AT 12:08Great rundown! I love how it breaks down the types in simple terms
Mike Rosenstein
October 19, 2025 AT 00:14Thank you for assembling such a thorough guide. It provides a solid foundation for readers who are beginning to explore audiology, and the clear headings make the complex information accessible.
BJ Anderson
October 20, 2025 AT 09:34The sheer audacity of ignoring the psychological impact of hearing loss in a so‑called 'complete' guide is staggering. It reduces a profoundly personal struggle to a sterile list of audiological terms, leaving sufferers feeling invisible.
Alexander Rodriguez
October 22, 2025 AT 00:28In short, if you have fluid in the middle ear, cleaning won’t fix it-you need medical treatment.
Abhinav Sharma
October 23, 2025 AT 18:08Remember, hearing is not just a physical sense; it connects us to the world like a bridge of vibrations 🌉. Embrace the journey of discovery, and let technology be the lantern guiding you through the silence 🕯️.
Vishnu Raghunath
October 25, 2025 AT 06:14Oh sure, because everyone’s favorite pastime is scheduling an audiogram after a night of loud concerts.
Aparna Dheep
October 26, 2025 AT 20:08One must appreciate the subtle elegance of otologic nomenclature, though the layperson may find such lexical flourishes bewildering.
Edward Glasscote
October 28, 2025 AT 13:48Thanks for the clear overview.
Gaurav Joshi
October 29, 2025 AT 23:08Contrary to the article’s optimism, many patients never receive proper follow‑up, rendering these recommendations moot.
Jennifer Castaneda
October 31, 2025 AT 11:14The guide succeeds in outlining the major categories of hearing loss, yet it overlooks the socioeconomic barriers that limit access to hearing aids. Addressing cost, insurance coverage, and availability of specialists would provide a more holistic picture of the challenges patients face.
Annie Eun
November 2, 2025 AT 02:08What about the role of early childhood screening programs in preventing long‑term deficits? Could universal audiometry in schools reshape our epidemiological landscape?
Jay Kay
November 3, 2025 AT 19:48Honestly, if you’re dealing with conductive loss, a simple tympanostomy tube can do wonders-no need for fancy tech.
Franco WR
November 5, 2025 AT 07:54I completely understand how overwhelming the flood of terminology can feel, especially when you’re trying to make sense of your own hearing health.
First, it helps to separate the categories: conductive issues often have a clear physical cause, like fluid or wax, which can sometimes be resolved quickly.
Second, sensorineural loss, while more permanent, offers a range of amplification options that have improved dramatically over the past decade.
Third, mixed loss simply combines these challenges, meaning a coordinated approach is essential.
Moreover, don’t underestimate the power of environmental modifications-quieting background noise and using assistive listening devices can make a huge difference day‑to‑day.
Finally, remember that regular check‑ups allow your audiologist to fine‑tune settings as your hearing changes, keeping you connected to the world around you.
Rachelle Dodge
November 6, 2025 AT 22:48Think of hearing as a kaleidoscope; each frequency adds a hue to your sonic world.
april wang
November 8, 2025 AT 16:28The distinction between conductive and sensorineural loss is not merely academic; it directly informs the therapeutic pathway.
Conductive loss, originating in the outer or middle ear, often presents with a classic “muffled” quality that improves markedly once the obstruction is removed.
Common culprits include cerumen impaction, otitis media with effusion, and ossicular chain discontinuity, each of which has a well‑established medical or surgical remedy.
By contrast, sensorineural loss stems from damage to the delicate hair cells of the cochlea or the auditory nerve itself, and this damage is typically irreversible.
Consequently, the primary interventions for sensorineural deficits are amplification devices such as digital hearing aids or, in more severe cases, cochlear implants.
Mixed loss combines elements of both, requiring a staged approach that first addresses any reversible conductive component before fitting amplification for the neural deficit.
Accurate diagnosis hinges on a battery of tests, beginning with pure‑tone audiometry to map thresholds across frequencies.
Tympanometry then evaluates middle‑ear pressure, discerning fluid or eustachian tube dysfunction that would point toward a conductive element.
Otoacoustic emissions and auditory brainstem responses add further granularity, distinguishing cochlear from neural pathologies.
Once the audiogram and ancillary studies are interpreted, a collaborative treatment plan can be formulated with the patient’s lifestyle goals in mind.
For individuals whose occupations expose them to high decibel environments, custom‑molded earplugs and regular monitoring are indispensable preventive measures.
Pediatric patients, meanwhile, benefit from early intervention programs that integrate speech‑language therapy with appropriate amplification.
It is also crucial to address comorbidities such as tinnitus, which often accompany sensorineural loss and may require dedicated management strategies.
Technological advances have yielded hearing aids with sophisticated noise‑reduction algorithms, directional microphones, and Bluetooth connectivity, vastly improving real‑world usability.
Finally, regular follow‑up appointments allow for fine‑tuning of device settings and early detection of any progressive changes in hearing thresholds.
In sum, a methodical, evidence‑based approach that tailors diagnosis and therapy to the specific type of loss empowers patients to maintain communication, safety, and quality of life.
Ada Xie
November 10, 2025 AT 04:34The article’s exposition is commendable; however, it would benefit from a more precise delineation between conductive and sensorineural etiologies, particularly concerning the pathophysiological mechanisms involved.
Stephanie Cheney
November 11, 2025 AT 19:28It is encouraging to see such a comprehensive resource; readers who follow the outlined steps are likely to experience meaningful improvements in their auditory health.