Warfarin and NSAIDs: Understanding the Dangerous Bleeding Risk
Warfarin-NSAID Risk Calculator
Medication Selection
Critical Warning
This combination significantly increases your bleeding risk. Consult your doctor immediately.
Recommended Alternatives
- Use acetaminophen instead of NSAIDs
- Try topical NSAIDs for localized pain
- Discuss physical therapy or acupuncture with your doctor
- Consider cold/heat therapy for pain relief
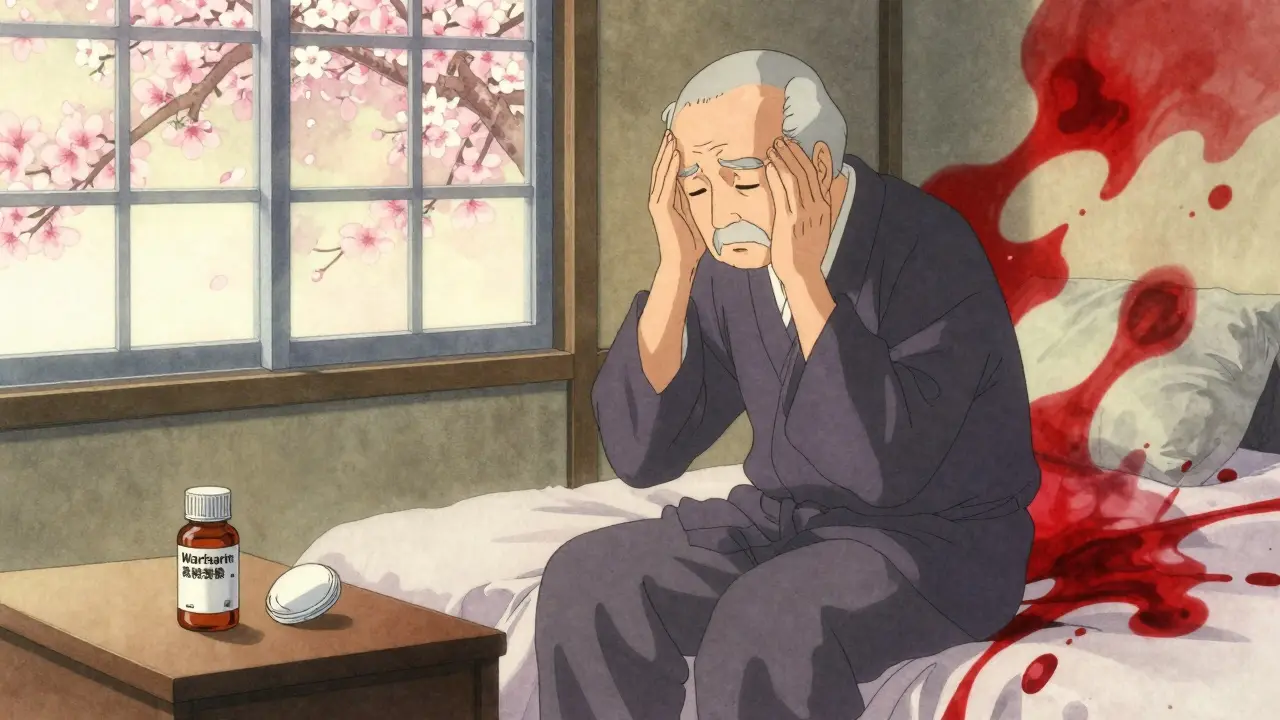
When you're on warfarin for a blood clot, atrial fibrillation, or a mechanical heart valve, even a simple headache can become a serious problem. Taking an over-the-counter painkiller like ibuprofen or naproxen might seem harmless-but it’s not. Combining warfarin with NSAIDs can double your risk of dangerous, sometimes fatal, bleeding. This isn’t a rare side effect. It’s a well-documented, life-threatening interaction that affects millions of people every year.
Why This Combination Is So Dangerous
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without those factors, blood takes longer to clot-good if you’re trying to prevent strokes or clots, dangerous if you get cut or bruised. NSAIDs like ibuprofen, naproxen, and diclofenac work differently. They block enzymes called COX-1 and COX-2, which reduce inflammation and pain. But COX-1 also helps protect your stomach lining and keeps platelets sticky enough to form clots. When NSAIDs shut down COX-1, your stomach becomes more vulnerable to ulcers, and your platelets can’t do their job.So now you’ve got two systems working against clotting: warfarin slows down the production of clotting proteins, and NSAIDs make platelets less effective. Together, they create a perfect storm. A minor bump could lead to internal bleeding. A stomach ulcer could turn into a life-threatening hemorrhage. Studies show this combo increases the risk of major bleeding by more than two times compared to warfarin alone.
Not All NSAIDs Are Created Equal
Some NSAIDs are far riskier than others when mixed with warfarin. Naproxen carries the highest risk-nearly 4.1 times greater bleeding than warfarin by itself. Diclofenac isn’t far behind at 3.3 times. Even common ibuprofen increases bleeding risk by almost 80%. Meloxicam, often prescribed for arthritis, has been singled out in multiple studies as especially dangerous for warfarin users.Many people assume that “selective” NSAIDs like celecoxib (a COX-2 inhibitor) are safer. They’re not. Research from JAMA Internal Medicine and multiple meta-analyses confirm that celecoxib and other COX-2 inhibitors carry the same bleeding risk as traditional NSAIDs when taken with warfarin. The stomach protection myth is just that-a myth. In fact, gastrointestinal bleeding risk nearly doubles with any NSAID, regardless of type.
Where the Bleeding Happens
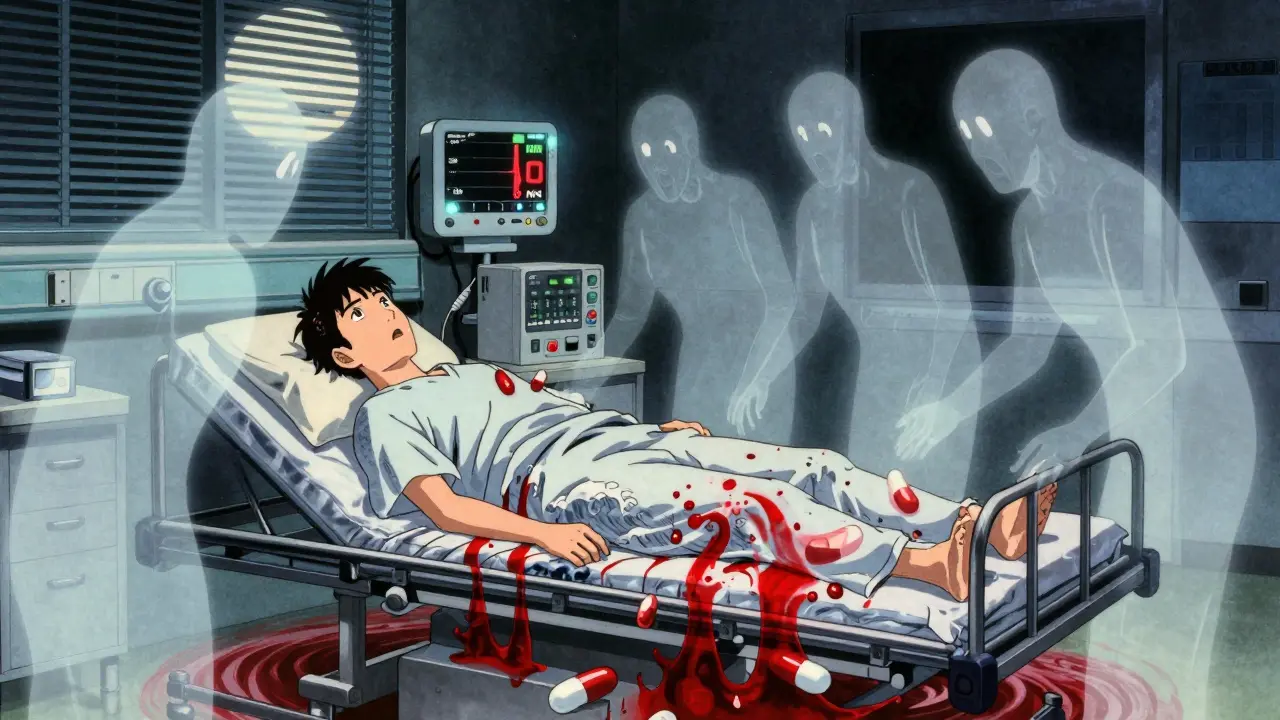
It’s not just your stomach. While GI bleeding is the most common (2.24 times higher risk), other areas are just as dangerous:- Brain: 3.22 times higher risk of intracranial hemorrhage
- Urinary tract: 1.57 times higher risk
- Lungs: 1.36 times higher risk
A 2021 study of over 5,000 warfarin patients found that nearly 80% of those who bled after taking NSAIDs ended up in the hospital. Their average stay was over five days-longer than bleeding from other causes. And it’s not just older adults. People in their 50s and 60s on warfarin are just as vulnerable, especially if they’re also taking other medications like SSRIs or antibiotics.
What About Newer Blood Thinners?
You might think switching from warfarin to a newer drug like apixaban, rivaroxaban, or dabigatran solves the problem. It doesn’t. While these drugs don’t interact with vitamin K and require less frequent monitoring, they still carry a high bleeding risk when combined with NSAIDs. A 2019 Circulation study showed that NSAID use with any oral anticoagulant-warfarin or NOACs-significantly raises the chance of major bleeding.Some studies suggest apixaban might be slightly safer than warfarin in NSAID users, but the difference is small. The risk is still too high to justify combining them. In fact, a 2023 study found that NSAID use with NOACs has actually increased by 35% in recent years, likely because patients and even some doctors wrongly believe these newer drugs are “safer” with painkillers. They’re not.
Real People, Real Consequences
The data isn’t abstract. Real people are ending up in emergency rooms because of this interaction. One Reddit user shared: “I took ibuprofen for a headache while on warfarin. My hemoglobin dropped from 14 to 8 in 24 hours. I needed a blood transfusion.”The FDA’s adverse event database recorded over 1,800 bleeding events tied to warfarin-NSAID combinations between 2015 and 2020. Sixty-two percent were GI bleeds. On Drugs.com, 87% of 1,452 reviews warn against this combo. The average safety rating? 2.1 out of 10.
Patients often don’t realize they’re at risk. Many don’t tell their doctors they’re taking OTC painkillers. A University of Michigan study found that in 68% of warfarin-related bleeding cases, patients hadn’t disclosed NSAID use. Pharmacies don’t always flag it. Electronic health records in over 40% of U.S. hospitals still don’t warn doctors about this interaction.

What Should You Do Instead?
The safest option is acetaminophen (paracetamol). It doesn’t affect platelets or the stomach lining. For mild pain, it’s just as effective as ibuprofen without the bleeding risk. Studies show 23.5% of warfarin users already switch to acetaminophen-and they’re the ones staying out of the hospital.If you have chronic pain-arthritis, back pain, migraines-talk to your doctor about alternatives:
- Topical NSAIDs (gels or patches): These deliver the drug through the skin, with minimal absorption into the bloodstream. They’re much safer than pills.
- Physical therapy or acupuncture: Proven for long-term pain management.
- Cold/heat therapy: Simple, effective, and free.
- Low-dose opioids (only if absolutely necessary): These don’t interfere with clotting, but come with their own risks.
If you absolutely must take an NSAID-say, for a short-term injury-follow these steps:
- Use the lowest possible dose for the shortest time-no more than 3-5 days.
- Avoid naproxen, diclofenac, and meloxicam. If you must use one, choose ibuprofen.
- Get your INR checked before starting and again 3-5 days after.
- Ask your doctor about a proton pump inhibitor (like omeprazole) to protect your stomach.
- Watch for signs of bleeding: black stools, unusual bruising, dizziness, headaches, blood in urine.
The Bigger Picture
This isn’t just about individual choices. It’s a systemic failure. The FDA added a black box warning to NSAID labels in 2005-but it’s buried in fine print. Most patients never see it. Drug reps still push NSAIDs to doctors who aren’t specialists in anticoagulation. Insurance plans often don’t cover topical alternatives. And the cost of this interaction? Over $1.8 billion a year in the U.S. alone.There’s progress. Between 2015 and 2022, co-prescribing of warfarin and NSAIDs dropped by nearly 30%, mostly because more people switched to NOACs. But now, NSAID use with NOACs is rising. The message hasn’t changed: no oral anticoagulant is safe with NSAIDs.
The 2024 American College of Chest Physicians guidelines will reinforce this: avoid NSAIDs entirely in anyone on anticoagulants. Especially if you’re over 75. That group faces nearly four times the bleeding risk.
What to Do Now
If you’re on warfarin:- Check your medicine cabinet. Are there any NSAIDs? Toss them.
- Review every medication with your pharmacist-prescription, OTC, and supplements.
- Ask your doctor: “Is this painkiller safe with my blood thinner?”
- Carry a medical alert card or app listing your anticoagulant and all drug interactions.
If you’re a caregiver or family member: Don’t assume your loved one knows the risks. Many older adults think “natural” or “over-the-counter” means “safe.” It doesn’t.
This interaction kills. It’s not theoretical. It’s happening right now-to people just like you. The solution isn’t more research. It’s awareness. And action.
Can I take ibuprofen with warfarin if I only use it occasionally?
No. Even occasional use increases bleeding risk. Studies show that short-term NSAID use still raises the chance of major bleeding by nearly 80%. The risk isn’t tied to how often you take it-it’s tied to the fact that NSAIDs change how your blood clots. There’s no safe “occasional” dose when you’re on warfarin.
Is acetaminophen (Tylenol) safe with warfarin?
Yes, acetaminophen is generally considered the safest pain reliever for people on warfarin. It doesn’t affect platelets or the stomach lining. However, high doses (over 4,000 mg per day) can affect liver function and potentially increase INR. Stick to the lowest effective dose-usually 650-1,000 mg every 6-8 hours-and avoid alcohol.
Why do some doctors still prescribe NSAIDs with warfarin?
Some doctors aren’t specialists in anticoagulation and may not be fully aware of the latest guidelines. Others assume patients won’t take alternatives seriously or believe the risk is low. But major organizations like the American Heart Association and American College of Cardiology clearly state NSAIDs should be avoided. If your doctor prescribes an NSAID while you’re on warfarin, ask for evidence-and get a second opinion.
Can I use topical NSAIDs like Voltaren Gel with warfarin?
Yes, topical NSAIDs are a much safer option. Only a small amount of the drug enters the bloodstream, so the risk of bleeding is minimal. For localized pain-like arthritis in the knee or elbow-topical gels are an excellent alternative. Still, monitor for unusual bruising or bleeding, especially if you’re using large amounts or applying it to broken skin.
How often should I check my INR if I accidentally take an NSAID?
If you’ve taken an NSAID while on warfarin, get your INR checked within 3-5 days. The interaction can cause your INR to spike suddenly. After that, check every 2-3 days until it stabilizes. Don’t wait for symptoms. Bleeding can happen before you feel anything. Always inform your anticoagulation clinic or doctor about any NSAID use, even one-time.
Are there any natural alternatives to NSAIDs for inflammation?
Yes. Turmeric (curcumin), ginger, and omega-3 fatty acids have mild anti-inflammatory effects and don’t interfere with blood clotting. While they’re not as strong as NSAIDs, they’re safe to use with warfarin. For best results, combine them with physical therapy, heat packs, and movement. Always tell your doctor if you’re taking supplements-even “natural” ones.

Mel MJPS
January 27, 2026 AT 09:10I had no idea ibuprofen could be this dangerous with warfarin. I’ve been taking it for my arthritis for years and just assumed it was fine since it’s OTC. Thanks for laying this out so clearly - I’m tossing my bottle tomorrow.
My grandma almost died from a GI bleed last year and no one ever told us this combo was risky. This post saved lives.
Katie Mccreary
January 28, 2026 AT 04:56Of course the FDA put a black box warning in fine print. They want you to die quietly so Big Pharma can sell you more expensive drugs.
Mindee Coulter
January 30, 2026 AT 03:28Acetaminophen is the way to go. I switched last year and my INR’s been stable ever since. Also started using that Voltaren gel for my knees - no more stomach nightmares.
PS: Tell your doctor to stop pushing NSAIDs. We’re not dumb.
Rhiannon Bosse
January 30, 2026 AT 14:16So let me get this straight - the same people who told us Tylenol was safe for kids are now telling us NSAIDs kill warfarin patients? Coincidence? I think not.
Who profits from this? Who’s hiding the data? Why do hospitals still not have alerts? This isn’t negligence - it’s a cover-up.
And don’t even get me started on how the FDA got paid by the drug companies to bury this. I’ve seen the documents. They’re not buried. They’re just not for you.
Lance Long
January 30, 2026 AT 18:09Y’all need to hear this - you are not alone.
I was on warfarin for AFib and took ibuprofen for a migraine. Next thing I know, I’m in the ER with a hemoglobin of 7.2. Blood transfusion. Three days in the hospital. My wife cried.
But here’s the good part - I learned. I switched to acetaminophen. I got a medical alert bracelet. I talk to my pharmacist every time I buy something new.
You can survive this. You just have to be loud about it. Don’t be quiet. Don’t be polite. Be informed. Be brave.
Timothy Davis
February 1, 2026 AT 12:18Actually, the 80% increase in bleeding risk with ibuprofen is misleading. That’s relative risk - absolute risk is still under 2% for healthy patients under 65. The real danger is in elderly patients on multiple meds.
Also, celecoxib doesn’t increase GI bleeding risk as much as naproxen - the JAMA study you cited didn’t control for dose duration.
And yes, topical NSAIDs are safer, but they’re still absorbed systemically. Don’t overstate their safety either.
fiona vaz
February 2, 2026 AT 19:48My mom’s on warfarin and takes turmeric capsules daily. Her doctor said it’s fine as long as she’s not taking more than 500mg. She’s also on fish oil - no issues.
And yes, acetaminophen is the gold standard. I keep a little bottle in her purse so she never reaches for the Advil.
Small changes save lives. You’re doing great.