How Subarachnoid Hemorrhage Leads to Chronic Pain: Causes, Risks, and Management
Subarachnoid Hemorrhage Pain Risk Calculator
Risk Factor Assessment
This tool estimates your risk of developing chronic pain following subarachnoid hemorrhage based on key clinical factors. Enter your information below to get an assessment.
Your Risk Assessment
Key Recommendations:
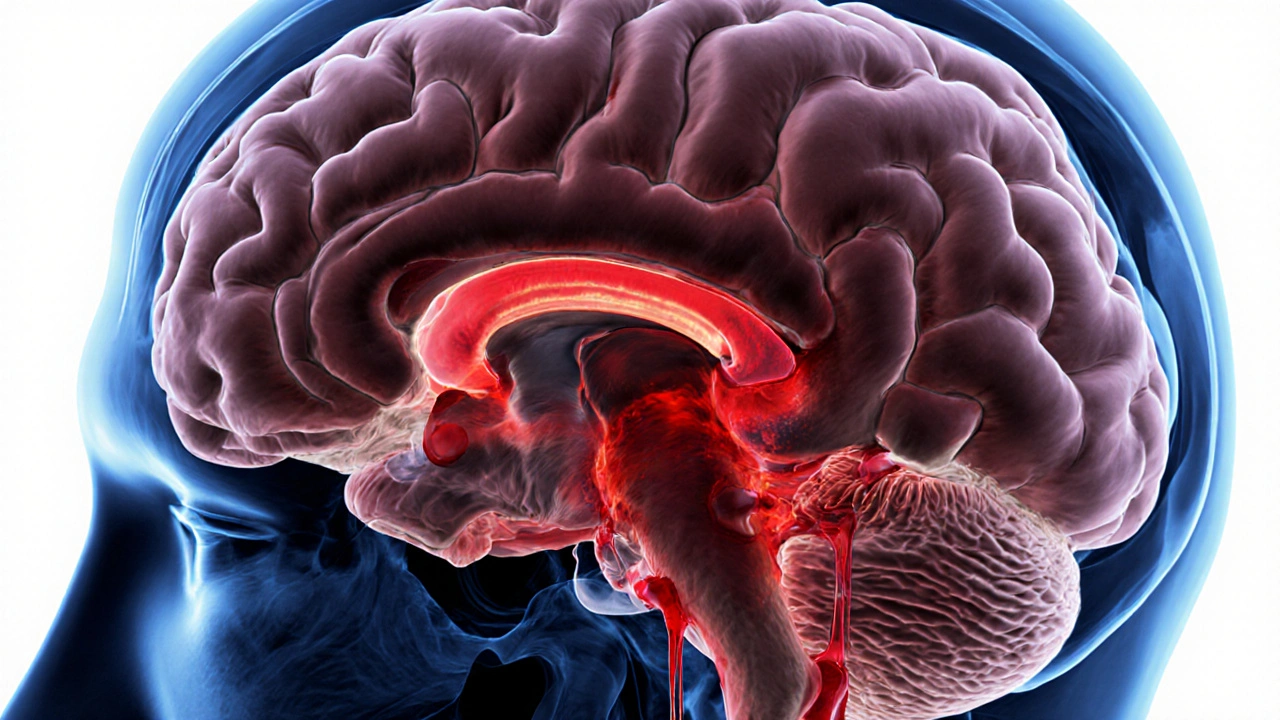
subarachnoid hemorrhage chronic pain may sound like an odd pairing, but the link is real and clinically important. When blood pools in the space surrounding the brain, the aftermath can turn into a lingering pain syndrome that follows patients for months or even years. This article breaks down why that happens, which patients are most at risk, and what you can do to lessen the burden.
Quick Take
- Subarachnoid hemorrhage (SAH) often triggers acute headache, but up to 30% develop chronic pain.
- Key drivers include cerebral vasospasm, nerve injury, and inflammatory cascades.
- Neuropathic pain patterns (burning, shooting) are common after SAH.
- Early rehab, targeted medication, and psychosocial support improve outcomes.
- Monitoring for vasospasm and treating it aggressively reduces long‑term pain risk.
Understanding Subarachnoid Hemorrhage
When blood leaks into the Subarachnoid Hemorrhage is a type of stroke caused by bleeding into the subarachnoid space surrounding the brain, it creates a sudden, severe headache often described as "the worst ever". Most cases stem from a ruptured cerebral aneurysm, although trauma or arteriovenous malformations can be culprits as well.
The immediate danger is increased intracranial pressure, reduced blood flow, and the risk of re‑bleeding. Modern neuro‑ICU care-rapid CT scanning, surgical clipping or endovascular coiling, and tight blood‑pressure control-has lowered mortality dramatically, but survivors frequently face long‑term challenges, including chronic pain.
What Is Chronic Pain After SAH?
Chronic pain is defined as any pain persisting beyond three months after the initial injury. In the SAH context, patients report a mix of headache, neck stiffness, and neuropathic sensations (tingling, electric‑shock‑like pain) that can impact daily activities and mood.
Studies from 2023‑2024 show that 20‑30% of SAH survivors report pain that meets chronic criteria, with neuropathic features in half of those cases. The pain often co‑exists with fatigue, cognitive fog, and depression, forming a complex syndrome that challenges both patients and clinicians.
Key Biological Triggers
Three major pathways link SAH to persistent pain:
- Vasospasm‑Induced Ischemia: Cerebral Vasospasm is the narrowing of brain arteries that commonly follows SAH, reducing blood flow to vulnerable nerve tissue. Reduced perfusion can damage trigeminal and cervical sensory pathways, priming them for chronic pain.
- Direct Nerve Injury: Blood‑borne inflammatory mediators irritate meningeal nociceptors and the trigeminovascular system. The resulting sensitization can become self‑sustaining, especially when the blood‑brain barrier remains compromised.
- Central Sensitization: Persistent activation of pain pathways reshapes spinal and brain circuitry, amplifying even mild stimuli. This phenomenon mirrors what we see in other post‑stroke pain syndromes.
Risk Factors to Watch
Not everyone with SAH ends up with chronic pain. Certain variables raise the odds:
- Aneurysm size and location: Larger anterior‑circle aneurysms tend to cause more extensive subarachnoid blood, raising inflammatory load.
- Severity of vasospasm: Measured by transcranial Doppler velocities, severe vasospasm (>200 cm/s) correlates with higher pain scores.
- Early opioid use: While opioids control acute headache, high‑dose or prolonged exposure can foster opioid‑induced hyperalgesia.
- Pre‑existing headache disorders: Migraine or tension‑type headache history predisposes to chronic pain after any brain insult.
- Poor psychosocial support: Depression, anxiety, and lack of rehab resources worsen pain perception.
Diagnosing the Pain
A thorough assessment starts with a detailed history: onset, quality, triggers, and relief measures. Use validated tools such as the Brief Pain Inventory and the Neuropathic Pain Scale to differentiate nociceptive from neuropathic components.
Imaging helps rule out delayed complications: repeat CT or MRI can identify hydrocephalus, scar tissue, or re‑bleeding that might mimic pain. When neuropathic features dominate, referral to a pain specialist for quantitative sensory testing can pinpoint the affected pathways.
Management Strategies
Effective pain control blends pharmacology, rehab, and psychosocial care.
Medication
- First‑line agents: Acetaminophen and NSAIDs for mild nociceptive pain.
- Neuropathic pain drugs: Gabapentin is an anticonvulsant that reduces neuronal excitability, often used for post‑stroke neuropathic pain or pregabalin, titrated slowly to minimize side effects.
- Tricyclic antidepressants: Low‑dose amitriptyline can help both pain and sleep.
- Opioid therapy: Opioid Therapy is generally reserved for breakthrough pain and used at the lowest effective dose for the shortest duration. Combine with non‑opioid agents to avoid dependence.
- Topical agents: Lidocaine patches for focal scalp or neck pain.
Rehabilitation
Rehabilitation is a multidisciplinary program that includes physical therapy, occupational therapy, and cognitive training aimed at restoring function after SAH. Early mobilization reduces muscle spasm, improves circulation, and may blunt central sensitization.
Specific exercises targeting neck and shoulder muscles alleviate tension‑type components, while gentle aerobic activity boosts endorphin release.
Interventional Options
- Botulinum toxin injections for refractory headache clusters.
- Occipital nerve block for scalp tenderness.
- Spinal cord stimulation in rare, severe neuropathic cases.
Psychosocial Support
Mind‑body therapies-cognitive‑behavioral therapy, mindfulness, and graded exposure-address the anxiety‑pain loop. Support groups for SAH survivors provide peer validation and practical coping tips.
Comparing Acute vs. Chronic Pain After SAH
| Aspect | Acute Pain | Chronic Pain |
|---|---|---|
| Onset | Minutes‑hours after bleed | Weeks‑months later |
| Quality | Throbbing, severe headache | Burning, shooting, or pressure‑type |
| Mechanism | Menigeal irritation, increased pressure | Vasospasm‑induced ischemia, neuropathic sensitization |
| Response to NSAIDs | Usually good | Often limited |
| Impact on daily life | Transient | Long‑term functional limitation |
Measuring Outcomes
Clinicians track pain using numeric rating scales (0‑10) and quality‑of‑life tools like the SF‑36. Improvements of ≥2 points on the pain scale or a 10% rise in SF‑36 scores are considered clinically meaningful.
Regular follow‑up at 1, 3, and 6 months post‑discharge helps catch evolving pain patterns early, allowing timely medication adjustments and rehab tweaks.
Future Directions
Research is exploring targeted anti‑inflammatory agents that could dampen the early cytokine surge after SAH, potentially preventing nerve sensitization. Neuroimaging biomarkers-functional MRI of the trigeminal nucleus-may soon predict which patients will develop chronic pain.
Genetic studies hint that polymorphisms in the COMT gene modulate pain susceptibility, opening the door for personalized therapy.
Key Takeaways for Patients and Caregivers
- Ask your neurologist about vasospasm monitoring; timely treatment lowers pain risk.
- Report any new or changing headache patterns, even months after discharge.
- Engage in early, supervised rehabilitation to keep muscles flexible and circulation robust.
- Don’t rely on opioids alone-combine with neuropathic agents and non‑pharmacologic methods.
- Seek mental‑health support if pain interferes with sleep or mood; emotional well‑being influences pain perception.

Frequently Asked Questions
Can a single bleed cause lifelong pain?
Yes, especially if the bleed triggers severe vasospasm or if the patient has pre‑existing headache disorders. Early intervention and rehab can reduce the likelihood, but some survivors do experience persistent pain for years.
What’s the difference between post‑SAH headache and chronic migraine?
Post‑SAH headache usually starts suddenly with the bleed and is linked to meningeal irritation. Chronic migraine follows typical migraine patterns (photophobia, aura) and may be independent of the hemorrhage. A thorough history helps differentiate them.
Are there non‑drug ways to ease pain after SAH?
Physical therapy, gentle aerobic exercise, mindfulness meditation, and cognitive‑behavioral therapy have all shown modest pain‑reducing effects. They work best when combined with appropriate medication.
How long should I stay on gabapentin after SAH?
Most clinicians taper gabapentin after 3‑6 months if pain scores improve. Sudden discontinuation can cause rebound pain, so any change should be gradual under medical supervision.
Is surgery ever needed just to treat pain?
Surgical options are rare. Decompression or removal of scar tissue may be considered if imaging shows a compressive lesion causing pain, but most cases are managed medically and through rehab.

Dawn Midnight
October 1, 2025 AT 13:26While the article correctly identifies vasospasm as a key driver, it should distinguish between “cerebral vasospasm” and “delayed cerebral ischemia,” which are not synonymous.
frank hofman
October 2, 2025 AT 07:22Yo, I think the whole “avoid opioids at all costs” vibe is overhyped 😂. Sure, they’ve got risks, but a short burst can actually curb that nasty post‑ bleed pain spike.
Dannii Willis
October 3, 2025 AT 01:18Great overview! I’d add that early multidisciplinary rehabilitation – especially physiotherapy focused on neck and shoulder mobility – can dramatically reduce the transition from acute headache to chronic neuropathic pain.
Robyn Du Plooy
October 3, 2025 AT 19:14The trigeminovascular system’s sensitisation after SAH is a classic example of neuroinflammatory cascade leading to hyperalgesia. When blood‑borne cytokines breach the blood‑brain barrier, they activate peripheral nociceptors, setting the stage for central sensitisation.
Angel Gallegos
October 4, 2025 AT 13:09Honestly, this reads like a textbook summary pasted into a blog.
ANTHONY COOK
October 5, 2025 AT 07:05Anyone reading this from overseas should know that American protocols for aggressive vasospasm management – triple‑H therapy, early endovascular spasmolysis – are the gold standard, and that’s why our outcomes are superior 😊.
Sarah Aderholdt
October 6, 2025 AT 01:01Healing after a bleed is not merely physiological; it’s an existential reclamation of agency, where each step of rehab reasserts the self’s narrative over pain.
Larry Douglas
October 6, 2025 AT 18:57The pathophysiology of chronic pain following subarachnoid hemorrhage is multifactorial and warrants detailed elucidation. Initial hemorrhagic insult precipitates a surge of inflammatory mediators such as interleukin‑6 and tumor necrosis factor‑alpha within the subarachnoid space. These cytokines facilitate peripheral nociceptor sensitisation, particularly of the trigeminal afferents innervating the meninges. Concomitantly, vasospasm may develop, reducing cerebral perfusion and inducing ischemic injury to nociceptive pathways. Ischemia further amplifies neuronal excitability through the accumulation of excitatory amino acids like glutamate. The resultant neuroplastic changes engender central sensitisation, a state in which dorsal horn neurons fire excessively to innocuous stimuli. Clinically, this manifests as a transition from the classic thunderclap headache to a persistent burning or shooting pain. Pharmacologic strategies must therefore address both peripheral and central mechanisms. First‑line agents such as acetaminophen and NSAIDs mitigate peripheral inflammation, whereas gabapentinoids attenuate calcium‑channel mediated neuronal firing. Tricyclic antidepressants, notably amitriptyline, are effective for the nocturnal component of neuropathic pain. Non‑opioid options are preferred, yet short courses of opioids may be justified for breakthrough pain when carefully monitored. Rehabilitation plays a pivotal role; early mobilization improves cerebrovascular autoregulation and reduces muscle tension that can exacerbate headache. Moreover, cognitive‑behavioral therapy has demonstrated efficacy in decoupling the affective dimension of pain. Ongoing research into targeted anti‑inflammatory agents and COMT gene profiling holds promise for personalised prophylaxis. Ultimately, a multimodal, patient‑centred approach remains the cornerstone of optimal long‑term outcomes.
Rakesh Manchanda
October 7, 2025 AT 12:52From a scholarly perspective, the integration of quantitative sensory testing with functional MRI could refine risk stratification beyond the current static calculators.
Erwin-Johannes Huber
October 8, 2025 AT 06:48Nice catch on the terminology you’re right about the distinction it helps clinicians stay precise and patients benefit from clear communication
Tim Moore
October 9, 2025 AT 00:44It is incumbent upon the neurocritical care team to implement a systematic protocol that encompasses vigilant vasospasm surveillance, judicious analgesic stewardship, and early initiation of multidisciplinary rehabilitation, thereby mitigating the incidence of chronic post‑hemorrhagic pain.
Erica Ardali
October 9, 2025 AT 18:40In the abyss of a ruptured artery, the brain cries out; yet we, mere mortals, must sculpt silence from that scream through science and will.
Justyne Walsh
October 10, 2025 AT 12:35Oh, because ignoring the obvious link between hemorrhagic trauma and persistent pain is such a brilliant way to keep patients suffering, isn’t it?
Callum Smyth
October 11, 2025 AT 06:31Exactly, and remember that each rehab session is a victory over that lingering pain narrative – keep pushing, the brain adapts.
Xing yu Tao
October 12, 2025 AT 00:27The epistemic pursuit of alleviating chronic post‑subarachnoid discomfort reflects humanity’s broader quest to transcend inherent vulnerability, a pursuit grounded in both empirical rigor and compassionate intent.
Adam Stewart
October 12, 2025 AT 18:23Just a gentle reminder to log any new headache patterns in your journal; subtle changes often herald the need for early intervention.
Selena Justin
October 13, 2025 AT 12:18We understand how overwhelming chronic pain can feel after such a life‑altering event; please reach out to your care team for tailored support and never hesitate to discuss your concerns.
Bernard Lingcod
October 14, 2025 AT 06:14The sarcasm underscores a truth that many clinicians overlook: the importance of proactive pain management cannot be overstated.